Association of Perceived Stress With Depression Among Vaccinated Healthcare Workers During the SARS-CoV-2 Variant Outbreak: The Mediating Role of Compassion Fatigue
Article information
Abstract
Objective
Depression was common during coronavirus disease-2019 (COVID-19) pandemic, while the association of perceived stress with depression among vaccinated healthcare workers has not been investigated. This study aimed to address this issue.
Methods
We included a total of 898 fully vaccinated healthcare workers during the outbreak of severe acute respiratory syndrome coronavirus 2 Delta variant in Nanjing, 2021. Depression was ascertained by Patient Health Questionnaire-9, with a cut-off score of ≥5 indicative of mild-to-severe depression. Perceived stress, resilience, and compassion fatigue were assessed by Perceived Stress Scale-10, Resilience Scale-25, and Professional Quality of Life Scale version-5, respectively. Logistic regression analyses were used to estimate the odds ratio (OR) and 95% confidence interval (CI), along with subgroup and mediation analyses.
Results
The prevalence of mild-to-severe depression was 41.1% in vaccinated healthcare workers. The odd of mild-to-severe depression was increased with higher perceived stress. Compared with vaccinated healthcare workers with the lowest tertile of perceived stress, those with the highest tertile had increased odds of mild-to-severe depression by 120% (OR 2.20, 95% CI 1.46 to 3.31) after multivariable-adjustment. However, perceived stress was not associated with mild-to-severe depression in vaccinated healthcare workers with strong resilience, but was in those with weak resilience (pinteraction=0.004). Further analysis showed that compassion fatigue mediated the relationship between perceived stress and mild-to-severe depression, with a mediating effect of 49.7%.
Conclusion
Perceived stress was related to an increased odd of mild-to-severe depression in vaccinated healthcare workers during COVID-19 pandemic, and this relationship might be explained by compassion fatigue.
INTRODUCTION
Coronavirus disease-2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has emerged as the most significant global health crisis since the influenza pandemic of 1918. As of December 2021, it is estimated that 18.2 million people had died worldwide based on the weekly-or monthly-reported mortality data from 74 countries and territories and 266 subnational locations [1]. However, the global number of death attributable to SARS-CoV-2 may continue to increase due to the rapidly growing number of infected patients from Delta and/or Omicron variants, which exhibited increased infectivity than Alpha variant [2,3].
Accumulating evidence has shown that depression is common during the pandemic, in particular in individuals infected with COVID-19 [4-6]. Studies have also suggested that healthcare workers, such as physicians and nurses, are at a high risk of depression [7,8]. A recent systematic umbrella review of the global evidence including 169,157 healthcare workers from 35 countries showed that the prevalence of depression in healthcare workers ranged from 17.9% to 36% during the COVID-19 pandemic [9]. However, results from the included individual studies in this review have seldomly accounted for whether healthcare workers had received COVID-19 vaccines [10,11], which are proved to protect against hospitalization and decrease the risk of death from COVID-19, thereby reducing the psychological burden to some extent.
Previous studies have extensively assessed the influencing factors on depression from COVID-19, such as sex, age, marital status, education levels, and family support, in healthcare workers [12-14]. However, few of them have focused on the contributing role of perceived stress, a psychological state that is occurred when the pressure exceeds the perceived ability of an individual to deal with [15,16], to depression in healthcare workers during the COVID-19 pandemic [17].
Being correlated with perceived stress, compassion fatigue refers to a state of tension or a sense of dissatisfaction resulted from cumulative exposure to repeated interactions that require high levels of empathy with distressed people [18,19]. Recent studies have shown that compassion fatigue is common in healthcare workers during the COVID-19 pandemic, because of their frequent contacts with distressed patients who are in need of care and the unpleasant patient situations [20]. However, it remains unclear whether compassion fatigue plays any role in the association of perceived stress with depression symptoms in vaccinated healthcare workers during the COVID-19 pandemic, given that compassion fatigue is associated with depression [21] while improvements in compassion fatigue may help to ameliorate depression symptoms in healthcare professionals [22].
Unlike compassion fatigue, resilience reflects the capacity of an individual in coping with adversity, traumatic, and stressful events [23,24]. A recent study observed a protective role of resilience against anxiety in Italian healthcare workers during the COVID-19 pandemic [25]. However, no studies have assessed whether resilience has any moderating effect for the association between perceived stress and depression.
Given these, and in order to assist in optimizing the management approaches for possible depression resulted from COVID-19, this study was primarily conducted to assess the association of perceived stress with depression, and secondarily to evaluate the mediating role of compassion fatigue as well as the moderating role of resilience in vaccinated healthcare workers during the COVID-19 pandemic.
METHODS
Study design and participants
This cross-sectional study was conducted from 14 August to 14 September 2021, when SARS-CoV-2 Delta variant outbroke in Nanjing that substantially affected the daily lives of the citizens (e.g., passengers planning to leave Nanjing by train had to present negative nucleic acid testing results taken within 48 hours) (https://www.chinadaily.com.cn/a/202107/27/WS60ffb523a310efa1bd664bd0.html). Completely vaccinated healthcare workers against COVID-19, such as doctors, nurses, pharmacists, radiologists, and physiotherapists, in Zhongda hospital, Southeast University, were consecutively invited to participate in this study via e-posters distributed by WeChat mobile application. The study protocol was approved by the Ethics Committee of Zhongda hospital, Southeast University (approval No. IRB 2021ZDSYLL196P01), and electronic informed consent was obtained from all participants. This study was reported according to the Strengthening the Reporting of Observational st-udies in Epidemiology guideline.
A web-based survey using a standard questionnaire designed in Wenjuanxing was sent to all participants through the WeChat mobile application. Participants were invited to respond to the questionnaire by scanning the quick response code, which had to be completed within one week. All questionnaires were anonymous, and no personal identities were disclosed in this survey. In order to ensure the quality of this survey, we excluded participants who finished the questionnaire <3 or >60 min. We also excluded participants who had received anti-depression treatment.
Data collection
In this study we collected information on demographic variables, personal information, depressive symptoms, perceived stress, compassion fatigue, and resilience. Demographic variables and personal information included sex (male and female), age, marital status (unmarried, married, and divorced/widow), education level (bachelor and below, master and doctor), occupation (doctors, nurses, and health-related administrators), contract employee, smoking, drinking, physical activity, and length of working years.
Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) [26-28], which comprises 9 items with the total scores between 0 and 27. For the PHQ-9 score, 1 to 4 is considered as minimal depression, 5 to 9 as mild depression, 10 to 14 as moderate depression, 15 to 19 as moderately severe depression, and 20 to 27 as severe depression [27]. In this study we defined the PHQ-9 score ≥5 as mild-to-severe depression for the primarily analysis, and ≥10 indicative of major depression (moderate-to-severe depression) for the secondary analysis [27,28]. The Cronbach’s alpha coefficient for PHQ-9 was 0.91 in this study.
Perceived stress was evaluated using the Perceived Stress Scale-10 (PSS-10), a short form of PSS that is used to measure how stressful an individual perceives events in his/her daily life [29]. PSS-10 contains 6 negative items used to assess the lack of control and negative affective reactions, and 4 positive items to reflect the ability to cope with existing stressors. Each item was rated on a 5-point scale from 0 (never) to 4 (always), with a high total score indicative of a high perceived stress level. The Cronbach’s alpha coefficient for PSS-10 was 0.83 in this study.
Compassion fatigue was assessed using the Chinese version of the Professional Quality of Life Scale version-5 (PROQOL-5) [30,31]. PROQOL-5 is consisted of 30 items based on a 5-point Likert scale, and has 3 subscales including compassion satisfaction, burnout, and secondary traumatic stress. For PROQOL-5, compassion fatigue referred to the subscales of burnout and secondary traumatic stress suggested by previous studies [32,33]. In this study the Cronbach’s alpha coefficients for burnout and secondary traumatic stress were 0.80 and 0.84, respectively.
Resilience was assessed using the Resilience Scale-25 (RS-25) [34]. RS-25 is comprised of 25 items and each item includes 7-point scale responses ranging from 1 (not agree at all) to 7 (fully agree). The answers were summed up together, with a high score representing a high resilience level. The Cronbach’s alpha coefficient for the RS-25 was 0.97 in this study.
Statistical analyses
Continuous variables are expressed as means±standard deviations (SDs) and categorical variables as numbers (percentages). Group differences based on the presence of mildto-severe depression were compared using the t-test or chisquared test. Logistic regression analyses were conducted to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) for mild-to-severe depression in relation to perceived stress based on the following models: model 1, crude model; model 2, adjusted for age and sex; and model 3, further adjusted for body mass index, education level, regular physical activity (yes or no), smoking (yes or no), contract employee (yes or no), daily working hours (8 hours above or not), compassion fatigue, and resilience. A test for linear trend was conducted with the use of tertiles of the PPS-10 scores as a continuous variable.
Subgroup analyses of sex (male vs. female), overweight/obesity (yes vs. no), regular physical activity (yes vs. no), contract employee (yes vs. no), and resilience level (strong vs. weak) were performed, and possible interactions were tested by incorporating the perceived stress-by-subgroup in model 3. We also performed a supplemental analysis to assess the relationship of major depression (PHQ-9 score ≥10) with perceived stress [27] to show the robustness of our primary analysis. Mediation analysis based on the generalized structural equation model was employed to evaluate the mediating effect of compassion fatigue in the relationship between perceived stress and mild-to-severe depression. A p<0.05 (twotailed) was considered statistically significant. All analyses were performed using Stata 14.0 software (StataCorp LP, College Station, TX, USA).
RESULTS
Characteristics of enrolled participants
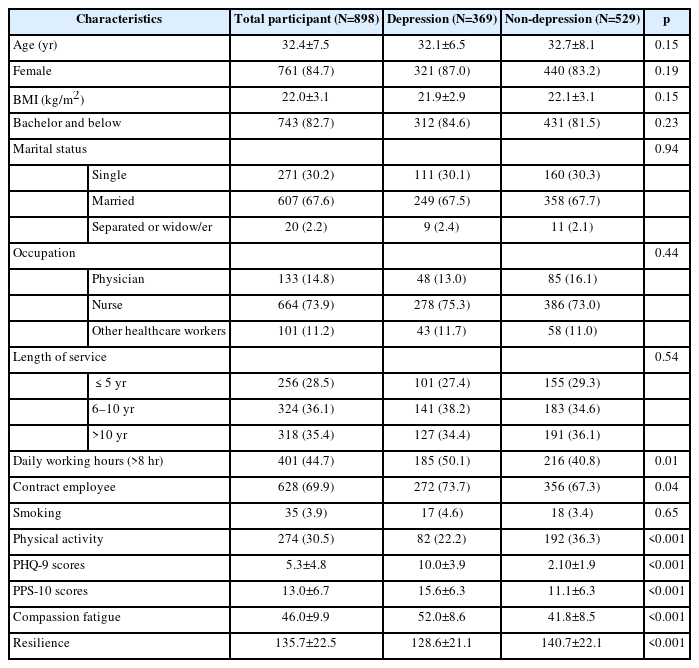
Of the 989 vaccinated healthcare workers surveyed, 71 were excluded due to the missing information on age or PHQ-9 score, and 20 because of receiving anti-depression treatment, leaving 898 eligible for inclusion in the present study (Supplementary Figure 1 in the online-only Data Supplement). The mean age of the included healthcare workers were 32.4±7.5 years, with 84.7% being females. A total of 369 (41.1%) healthcare workers had mild-to-severe depression; and among them, 135 (15.0%) had major depression. Healthcare workers with mild-to-severe depression were likely to have more daily working hours, less physical activity, a larger percentage of contract employees, higher levels of perceived stress and compassion fatigue, and lower levels of resilience, compared with those without (p<0.05) (Table 1).
The association between perceived stress and depression
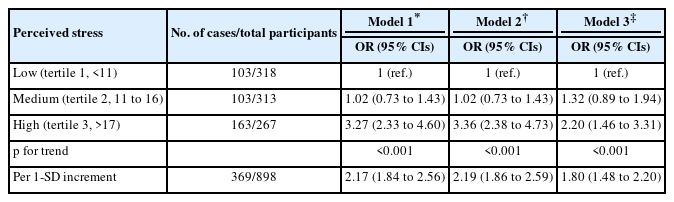
The association between perceived stress and the odd of mild-to-severe depression is presented in Table 2. The odd of mild-to-severe depression was increased with increments in perceived stress (models 1–3, p<0.001). Compared with vaccinated healthcare workers with the lowest tertile of perceived stress, those with the highest tertile had an OR of mildto-severe depression as 3.27 (95% CI 2.33 to 4.60) in model 1. However, the association was attenuated to be 2.20 (95% CI 1.46 to 3.31) in model 3. Further analysis showed that the OR of mild-to-severe depression was 1.80 (95% CI 1.48 to 2.20) per 1-SD increment in PSS-10 scores model 3. Supplemental analysis for major depression showed a similar outcome, with the ORs ranging from 2.08 to 2.67 per 1-SD increment in PSS-10 scores in different adjustment models (Supplementary Table 1 in the online-only Data Supplement).
Subgroup analyses showed that the association between perceived stress and mild-to-severe depression was not sig nificantly affected by sex, body weight status, physical activity, and the types of employment (pinteraction≥0.33) (Table 3). However, perceived stress was not related to an increased OR of mild-to-severe depression in healthcare workers with strong resilience, but was in those with weak resilience (pinteraction=0.004) (Table 3).
Mediating role of compassion fatigue
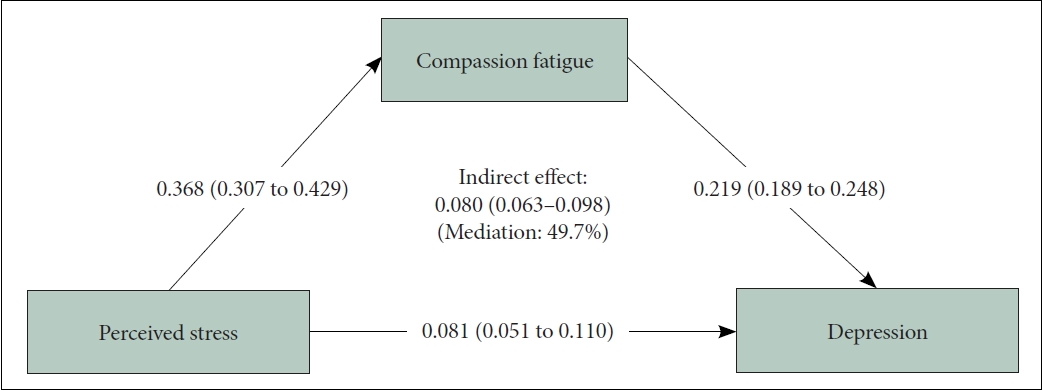
Mediation analysis on the role of compassion fatigue in the association of perceived stress with mild-to-severe depression is shown in Figure 1. Results showed that compassion fatigue significantly mediated the relationship between perceived stress and mild-to-severe depression, with the mediating effect being 49.7%.
DISCUSSION
Main findings
This survey is the first cross-sectional study that focused on the association of perceived stress with mild-to-severe depression among vaccinated healthcare workers during the COVID-19 pandemic. In this study, we found that about 41% vaccinated healthcare workers had mild-to-severe depression. Higher perceived stress was associated with a lower odd of mild-to-severe depression, and this association might be moderated by resilience. We also found that compassion fatigue may mediate the association of perceived stress with mild-tosevere depression by approximately 50%.
Interpretations and implications
Our study showed that the odd of mild-to-severe depression was increased by 80% per 1-SD increment in perceived stress among vaccinated healthcare workers after multivariable-adjustment during the SARS-CoV-2 Delta variant outbreak. This is in general consistent with the results from the study by Lee et al. [17], which showed that high perceived stress was associated with an increased PHQ-9 score in the Korean healthcare workers. However, that study did not account for the matter whether healthcare workers had received COVID-19 vaccines. There are some explanations for the association of perceived stress with depression. Prior studies showed that there was a significant genetic correlation between perceived stress and depression, indicating that these two constructs may share a common genetic basis [35,36]. As a result, participants who are vulnerable to high perceived stress might be also susceptible to an increased probability of depression. Furthermore, perceived stress was associated with unfavorable functional and structural changes in the prefrontal cortex, which may cause depressive symptoms, leading to depression subsequently [37,38].
Of note, although being vaccinated against COVID-19, we found that 41% of the healthcare workers had mild-to-severe depression, which was comparable to other studies conducted in the general healthcare workers (i.e., 36.2% with mildto-severe depression) or the general population (i.e., 33.7% with depression) [4,11], although their questionnaires used for assessing depression as well as the cut-off points for ascertaining depression varied (e.g., the Depression, Anxiety and Stress Scale-21, Beck Depression Inventory-II). This indicates that vaccine administration might be not able to sufficiently reduce the onset of mental problems in healthcare workers, in particular compared with the general population, at least for depression, during the SARS-CoV-2 Delta variant outbreak.
Our study also showed that increments in perceived stress were not associated with an increased odd of mild-to-severe depression in vaccinated healthcare workers with strong resilience, but were in those with weak resilience. Given this and considering that resilience may strengthen the resistance to stress by allowing greater access to positive emotional resources, it seems likely that improvements in resilience may help to offset the detrimental psychological effects from increased perceived stress, at least partly [39]. In addition, regular physical activity is considered effective in copying with perceived stress and associated with lower risk of depression [40-42]. However, in our study, we did not find that regular physical activity has any significant moderating effect for the association of perceived stress with mild-to-severe depression in vaccinated healthcare workers during the SARS-CoV-2 Delta variant outbreak. Moreover, neither sex nor body weight status affected this association, although there is evidence that depression is more common in females or among participants with obesity than their counterparts.
Furthermore, our mediation analysis showed that the impact of perceived stress on mild-to-severe depression could be partly mediated by compassion fatigue, with a mediating effect of about 50%. This is of significant clinical importance, since on the one hand it suggests that healthcare workers, who are prone to compassion fatigue when exposed to stressors from COVID-19, might have an increased odd of depression. On the other hand, it provides evidence in support of the notion that reducing compassion fatigue might assist in minimizing the negative impact from perceived stress on depression. Thus, programs designed to ease perceived stress and/or reduce compassion fatigue (e.g., mindfulness-based interventions [22]) are warranted to lower the occurrence of depression during the COVID-19 pandemic.
Strengths and limitations
This study, which is to our knowledge, the first analysis focused on the association of perceived stress with depression in vaccinated healthcare workers during the SARS-CoV-2 Delta variant outbreak, along with the exploration of mediating effect from compassion fatigue. However, our study has several limitations. First, the causal relationship between perceived stress and depression cannot be determined due to the nature of cross-sectional design. Future prospective cohort studies are warranted to validate our findings. Moreover, residual confounding could not be excluded because of some unmeasured factors (e.g., dietary intake). Second, psychosocial variables were mainly assessed using self-report questionnaires, which might be subject to recall and/or reporting bias. Third, the use of PHQ-9 score of ≥5 to define clinically meaningful depression might be challenged, since PHQ-9 score of 5–9 may largely represent depressive symptoms. However, our supplemental analysis, which employed the cut-off point of ≥10 to define depression, showed a comparable outcome that perceived stress was associated with depression among vaccinated healthcare workers. Nevertheless, we defined PHQ-9 score of ≥5 as mild-to-severe depression for better transparency in our study. Finally, participants in our study were recruited mainly from a single center, challenging their representativeness potentially.
Conclusions
In conclusion, two-fifths of the vaccinated healthcare workers had mild-to-severe depression during the SARS-CoV-2 Delta variant outbreak. Increments in perceived stress were related to elevated prevalence of mild-to-severe depression, but not in vaccinated healthcare workers with strong resilience. Moreover, the association of perceived stress with prevalent depression was partly explained by compassion fatigue. These findings suggest that easing perceived stress, enhancing resilience, and/or reducing compassion fatigue may help to cope with depression in vaccinated healthcare workers during the COVID-19 pandemic.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0238.
Perceived stress and the odd of major depression
Flow diagram for participants inclusion and exclusion. PHQ-9, Patient Health Questionnaire-9.
Notes
Availability of Data and Material
The data for the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Xue Cai, Guohong Li, Cuirong Xu, Yingzi Huang, Shanhu Qiu. Data curation: Xue Cai, Shanhu Qiu. Formal analysis: Xue Cai, Dan Luo, Cuirong Xu, Yingzi Huang, Shanhu Qiu. Methodology: Guohong Li, Haixia Feng, Xiaoyan Wang, Lijun He, Cuirong Xu. Project administration: Guohong Li, Haixia Feng, Xiaoyan Wang, Lijun He. Supervision: Cuirong Xu, Yingzi Huang. Validation: Dan Luo, Cuirong Xu, Yingzi Huang, Shanhu Qiu. Writing—original draft: Xue Cai, Dan Luo, Shanhu Qiu. Writing—review & editing: all authors.
Funding Statement
This work was partly supported by the scientific research project from the Chinese Nursing Association (grant no. ZHKYQ202117) and the Open Project Programme of the Key Base for Standardized Training for General Physicians in Southeast University (grant no. ZDZYJD-QK-2022-3). Shanhu Qiu has been supported by the “Best Young Scholars” Fellowship from Southeast University. The funders had no roles in the design of the study and collection, analysis, and interpretation of data or in writing the manuscript.