|
 |
- Search
| Psychiatry Investig > Volume 20(4); 2023 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Supplementary Materials
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Ji Sun Kim, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Bin-Na Kim, Ji Sun Kim. Formal analysis: Seul-Ah Lee, Simyang Heo. Investigation: Somin Kim, Chaeyeon Park, Yujin Jung, Garam Ji, Hyeon-Ah Lee, Kibum Kim, Sungkean Kim. Writing—original draft: Seul-Ah Lee, Simyang Heo. Writing—review & editing: Bin-Na Kim, Ji Sun Kim.
Funding Statement
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C0619).
Figure 1.
Table 1.
| Study | Study design | Sample size | Age (yr) | Country | Population | Setting | Intervention | Outcome measures | Comparator/control | Outcome (VR-based intervention) |
|---|---|---|---|---|---|---|---|---|---|---|
| Nijland et al. [45] (2021) | Within subject pre-post | 326 | Adult | Netherlands | ICU nurses of the UMCG working on one of the four intensive care units for COVID-19 patients | University Medical Centre Groningen (UMCG) | VR relaxation (VRelax) (≥10 min, actual use duration was not collected), including videos of calming natural environments | Perceived stress (VAS-stress: 0-100/PSS-10: 10 items, 5-point) | N/A | Mean VAS-stress before VRelax was 35.2 (standard deviation [SD]=24.3), mean VAS-stress after VRelax was 21.1 (SD=21.1). The mean difference was 14.0 points, SD=13.3; t-test value=8.6; p<0.005; 95% confidence interval (CI)=10.8-17.3. |
| Resilience (CD-RISC-10: 10 items, 5-point) | ||||||||||
| Riva et al. [47] (2021) | Within subject pre-post | 40 | ≥18 | Italy | People who had experienced at least two months of strict social distancing | Recruited through the combined use of traditional strategies and advertisements on a social media platform | VR video “The Secret Garden” (10 min, 1 week): immersive modality+non-immersive modality+a series of social exercises (1 week) | Anxiety and depression (DASS) | N/A | There was a significant effect of time for the primary outcomes of depression [F(3, 115.2)=6.68; p<0.001, η2 p=0.15, 95% CI (0.04, 0.26)], stress [F(3, 115.17)=6.35; p<0.001, η2 p=0.14, 95% CI (0.03, 0.25)], general distress [F(3, 115.15)=6.97; p<0.001, η2 p=0.15, 95% CI (0.04, 0.26)], perceived stress [F(3, 115.17)=5.15; p=0.002, η2 p=0.12, 95% CI (0.02, 0.22)], and hopelessness [F(3, 115.07)=4.80, p=0.003, η2 p=0.11, 95% CI (0.01, 0.21)]. No significant effect of time was found on anxiety [F(3, 115.2)=2.2556, p>0.05, η2 p=0.06, 95% CI (0.00, 0.14)]. |
| Perceived stress (PSS-10) | ||||||||||
| Hopelessness (BHS) | ||||||||||
| Regarding primary outcome measures, participants exhibited improvements from baseline to post-intervention for depression levels, stress levels, general distress, and perceived stress (all ps<0.05) but not for the perceived hopelessness (p=0.110). | ||||||||||
| Beverly et al. [44] (2022) | Within subject pre-post | 102 | ≥18 | USA | Frontline healthcare workers, including direct care providers, indirect care providers, and support or administrative services | OhioHealth Healthcare System (an emergency department, a medical/surgical unit, and a critical care unit) | Tranquil Cine-VR simulation (3 min, 1 session): depicted a lush, green nature preserve to promote relaxation and peace | Subjective stress (VAS-stress: 10-point) | N/A | A significant reduction in subjective stress scores from pre- to post-simulation (mean change=-2.2±1.7, t=12.749, p<0.001), with a Cohen’s d of 1.08, indicating a very large effect |
| Only four (3.9%) participants met the cutoff for high stress after the simulation, and the number of people with high stress differed pre- and post-simulation (χ2=8.582, p=0.003). | ||||||||||
| Participants who met the cutoff for high stress pre-simulation showed a greater reduction in subjective stress scores compared to participants who did not meet the cutoff pre-simulation (mean change=3.3±2.0 vs. 1.6±1.2, t=5.403, p<0.001). | ||||||||||
| Groenveld et al. [41] (2022) | Within subject pre-post | 48 | ≥16 | Netherlands | Patients with post COVID-19- condition referred for physiotherapy to a physiotherapists | Community-based practice or outpatient rehabilitation clinic | Multimodal VR exercises (30 min per session, 6 weeks): physical (SyncVR Fit), cognitive (Koji’s Quest), relaxation and distraction exercises (SyncVR Relax & Distract) | Anxiety and depression (HADS: ≥8) | N/A | The scores of the Positive Health questionnaire and SF-12 were significantly increased after 6 weeks. |
| Quality of life (SF-12, The Positive Health questionnaire) | The 1.4 points decrease of total HADS score was not significant (p=0.08) for the total group but reached significance (p=0.01) for the subgroup of patients who used the mental VR applications. | |||||||||
| Meyer et al. [46] (2022) | Within subject pre-post | 38 | ≥18 | Germany | People who had experienced at least two months of strict social distancing | N/A | Online self-help protocol “COVID Feel Good” | Depressiveness (DASS: 7 of 21 items, 4-point) | N/A | There was a statistically significant effect of the variable Time displaying difference between the 4 measurements (day -7, 0, 7, 21) for general distress [F(3, 111)=11.65, p<0.001, η2=0.061], perceived stress [F(3, 111)=4.74, p=0.004, η2=0.038], as well as the subscales depression [F(3, 111)=7.93, p≤0.001, η2=0.047], anxiety [F(3, 111)=7.80, p<0.001, η2=0.047], and stress [F(3, 111)=6.78, p<0.001, η2=0.052]. |
| VR video “Secret Garden” (10 min, 1 week)+daily social or cognitive exercise (1 week) | Anxiety (DASS: 7 of 21 items, 4-point) | |||||||||
| General distress (SUDS: 0-100) | ||||||||||
| Perceived stress (PSS-10: 10 items, 5-point/DASS: 7 of 21 items, 4-point) | ||||||||||
| Hopelessness (BHS: 20 items, true or false) | However, the decrease in hopelessness turned out to be insignificant [F(3, 111)=2.65, p=0.052, η2=0.009]. | |||||||||
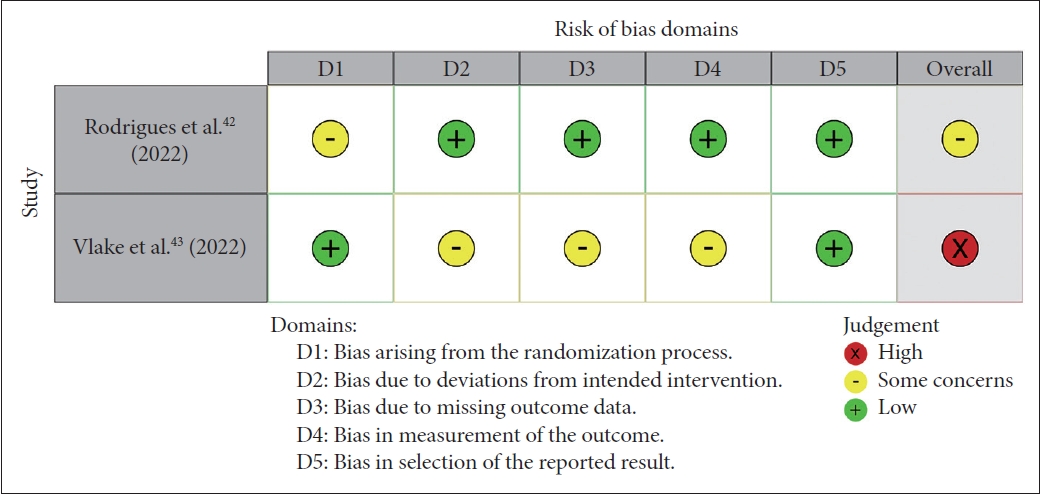
| Rodrigues et al. [42] (2022) | RCT | 44 (22+22) | 18-80 | Brazil | Enrolled from inpatient wards for patients with COVID-19 | Regional hospital or university hospital at four sites in Brazil | Therapeutic VR (10 min, 1 session): VR videos with images of landscapes and/or mindfulness techniques)+Occupational therapy (30 min, 1 session) | Anxiety and depression (HADS) | Non-therapeutic VR + Occupational therapy | Concerning the HADS scale, only the experimental group had a difference from baseline to post-intervention (anxiety: baseline 4.10±2.90, post 2.10±2.23, p=0.001, effect size=0.773245). |
| Vlake et al. [43] (2022) | RCT | 89 (45+44) | ≥18 | Netherlands | COVID-19 patients in ICU | A university teaching hospital and 3 universityaffiliated secondary care hospitals | ICU-VR (14 min, 1 session) consists of 6 scenes+60-minute-long consultation | PTSD (IES-R: ≥33) | Control (only consultation without VR intervention) | The prevalence and severity of psychological distress were limited throughout follow-up, and no differences in psychological distress or quality of life were observed between the groups. ICU-VR improved satisfaction with (mean score 8.7, SD 1.6 vs. 7.6, SD 1.6 [ICU-VR vs. control]; t64=-2.82, p=0.006) and overall rating of ICU aftercare (mean overall rating of aftercare 8.9, SD 0.9 vs. 7.8, SD 1.7 [ICU-VR vs. control]; t64=-3.25; p=0.002) compared to controls. |
| Anxiety (HADS: 7 items, ≥8) | ||||||||||
| Depression (HADS: 7 items, ≥8) | ||||||||||
| Quality of life (SF-36, EQ-5D) |
ICU, Intensive Care Unit; COVID-19, coronavirus disease-2019; VR, virtual reality; N/A, not available; VAS-stress, Visual Analogue Scale-stress; CD-RISC-10, 10-item Connor-Davidson Resilience Scale; DASS, Depression Anxiety Stress Scales; PSS-10, Perceived Stress Scale 10; BHS, Beck Hopelessness Scale; SF-12, Short Form-12; SUDS, Subjective Units of Distress Scale; HADS, Hospital Anxiety and Depression Score; IES-R, Impact of Event Scale-Revised; SF-36, Short-Form 36; EQ-5D, European Quality of Life 5 dimensions
Table 2.
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nijland et al. [45] (2021) | Y | Y | N | Y | CD | N | Y | NA | NA | Y | N | NA |
| Riva et al. [47] (2021) | Y | Y | N | Y | Y | Y | Y | NA | Y | Y | Y | NA |
| Beverly et al. [44] (2022) | Y | Y | N | Y | N | Y | N | N | NA | Y | N | NA |
| Groenveld et al. [41] (2022) | Y | Y | CD | Y | NR | N | Y | NA | N | Y | N | NA |
| Meyer et al. [46] (2022) | Y | Y | N | Y | Y | Y | Y | NA | NR | Y | Y | NA |
Q1: Was the study question or objective clearly stated?, Q2: Were eligibility/selection criteria for the study population prespecified and clearly described?, Q3: Were the participants in the study representative of those who would be eligible for the intervention in the general or clinical population of interest?, Q4: Were all eligible participants that met the prespecified entry criteria enrolled?, Q5: Was the sample size sufficiently large to provide confidence in the findings?, Q6: Was the intervention clearly described and delivered consistently across the study population?, Q7: Were the outcome measures prespecified, clearly defined, valid, reliable, and assessed consistently across all study participants?, Q8: Were the people assessing the outcomes blinded to the participants’ interventions?, Q9: Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis?, Q10: Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided p-values for the pre-to-post changes?, Q11: Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (i.e., did they use an interrupted time-series design)?, Q12: If the intervention was conducted at a group level (e.g., a whole hospital, a community, etc.) did the statistical analysis take into account the use of individual-level data to determine effects at the group level?. NIH, National Institutes of Health; Y, yes; N, no; CD, cannot determine; NA, not applicable; NR, not reported
REFERENCES