 |
 |
- Search
| Psychiatry Investig > Volume 20(9); 2023 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Supplementary Materials
Supplementary Figure 1.
Notes
Availability of Data and Material
The data are available on request from the corresponding author without any access criteria.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Che-Sheng Chu. Data curation: Mu-Hong Chen, Chih-Sung Liang. Formal analysis: Mu-Hong Chen. Funding acquisition: Che-Sheng Chu, Shu-Li Cheng. Investigation: Che-Sheng Chu, Chih-Sung Liang. Methodology: Mu-Hong Chen, Chih-Sung Liang. Project administration: Shih-Jen Tsai. Resources: Shih-Jen Tsai, Tzeng-Ji Chen. Software: Mu-Hong Chen, Chih-Sung Liang. Supervision: Mu-Hong Chen, Chih-Sung Liang. Validation: Ya-Mei Bai, Chih-Sung Liang. Visualization: Ya-Mei Bai, Fu-Chi Yang. Writing—original draft: Che-Sheng Chu. Writing—review & editing: all authors.
Funding Statement
The study was supported by grant from Taipei Veterans General Hospital (V106B-020, V107B-010, V107C-181, V108B-012), Kaohsiung Veterans General Hospital (KGVGH-110-051, VGHKS-109-070, KSVGH111-082, KSVGH111-181), Yen Tjing Ling Medical Foundation (CI-110-30) and Ministry of Science and Technology, Taiwan (107-2314-B-075-063-MY3, 108-2314-B-075-037, MOST-109-2314-B-075B-001-MY2) and MacKay Medical College, Taiwan (MMC-RD-111-1B-P003, for SLC). The funding source had no role in any process of our study.
Figure 1.
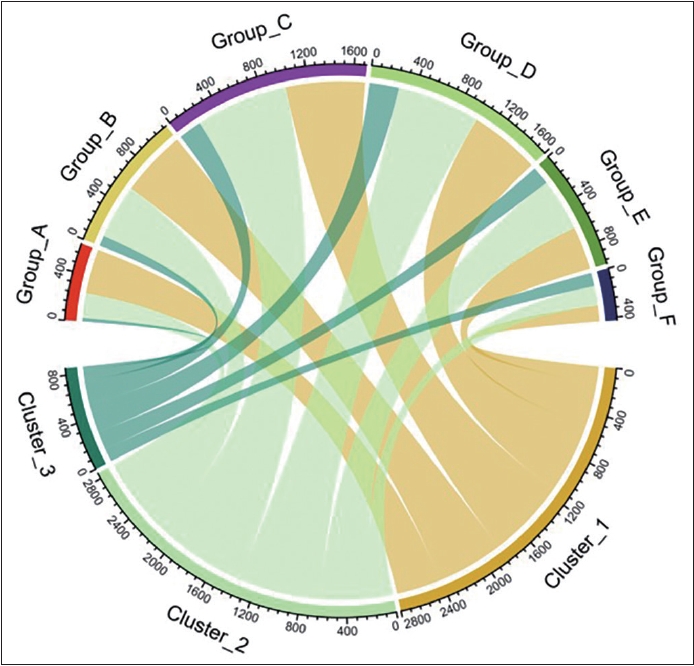
Figure 2.
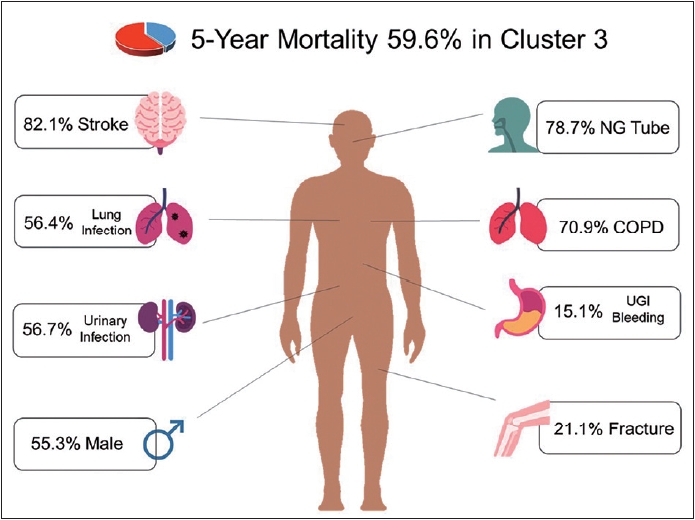
Table 1.
| Group A (N=635) | Group B (N=1,145) | Group C (N=1,701) | Group D (N=1,654) | Group E (N=995) | Group F (N=426) | p | Post hoc (Bonferroni) | |
|---|---|---|---|---|---|---|---|---|
| Age (yr) | 65-69 | 70-74 | 75-79 | 80-84 | 85-89 | ≥90 | ||
| Female | 368 (58.0) | 607 (53.0) | 858 (50.4) | 848 (51.3) | 563 (56.6) | 226 (53.1) | 0.003 | A>C*, C<E* |
| Stroke | 386 (60.8) | 696 (60.8) | 1,133 (66.6) | 1,127 (68.1) | 664 (66.7) | 273 (64.1) | <0.001 | A<D*, B<C*, B<D** |
| Bone fracture | 48 (7.6) | 67 (5.9) | 131 (7.7) | 212 (12.8) | 159 (16.0) | 98 (23.0) | <0.001 | A<D**, A<(E, F)***, B<(D, E, F)***, C<(D, E, F)***, D<F***, E<F* |
| Medical history | ||||||||
| PVD | 46 (7.2) | 83 (7.2) | 124 (7.3) | 138 (8.3) | 73 (7.3) | 30 (7.0) | 0.839 | |
| COPD | 232 (36.5) | 482 (42.1) | 854 (50.2) | 908 (54.9) | 536 (53.9) | 244 (57.3) | <0.001 | A<(C, D, E, F)***, B<(C, D, E, F)*** |
| Cancer | 104 (16.4) | 188 (16.4) | 363 (21.3) | 386 (23.3) | 220 (22.1) | 110 (25.8) | <0.001 | A<(D, F)**, B<(C, E)*, B<D***, B<F** |
| Diabetes | 314 (49.4) | 629 (54.9) | 904 (53.1) | 823 (49.8) | 435 (43.7) | 144 (33.8) | <0.001 | A>F***, B>(E, F)***, C>(E, F)***, D>E*, D>F***, E>F** |
| Dyslipidemia | 146 (23.0) | 286 (25.0) | 596 (35.0) | 616 (37.2) | 398 (40.0) | 170 (39.9) | <0.001 | A<(C, D, E, F)***, B<(C, D, E, F)*** |
| UGI bleeding | 23 (3.6) | 34 (3.0) | 90 (5.3) | 66 (4.0) | 51 (5.1) | 25 (5.9) | 0.015 | B<C* |
| Hypertension | 500 (78.7) | 974 (85.1) | 1,469 (86.4) | 1,435 (86.8) | 857 (86.1) | 368 (86.4) | <0.001 | A<(B, F)*, A<(C, D)***, A<E** |
| Lung infection | 21 (3.3) | 73 (6.4) | 148 (8.7) | 170 (10.3) | 111 (11.2) | 68 (16.0) | <0.001 | A<B*, A<(C, D, E, F)***, B<(D, E)**, B<F***, C<F**, D<F* |
| Nasogastric tube | 47 (7.4) | 135 (11.8) | 202 (11.9) | 220 (13.3) | 140 (14.1) | 89 (20.9) | <0.001 | A<B*, A<C**, A<(D, E, F)***, B<F***, C<F***, D<F**, E<F* |
| Urinary infection | 102 (16.1) | 184 (16.1) | 332 (19.5) | 326 (19.7) | 180 (18.1) | 99 (23.2) | 0.007 | B<F* |
| Myocardial infarction | 18 (2.8) | 38 (3.3) | 84 (4.9) | 81 (4.9) | 45 (4.5) | 16 (3.8) | 0.073 | |
| Chronic kidney disease | 61 (9.6) | 131 (11.4) | 196 (11.5) | 190 (11.5) | 107 (10.8) | 35 (8.2) | 0.295 | |
| Coronary artery disease | 316 (49.8) | 599 (52.3) | 995 (58.5) | 990 (59.9) | 584 (58.7) | 236 (55.4) | <0.001 | A<(C, E)**, A<D***, B<(C, E)*, B<D** |
| Congestive heart failure | 100 (15.7) | 214 (18.7) | 416 (24.5) | 461 (27.9) | 269 (27.0) | 137 (32.2) | <0.001 | A<(C, D, E, F)***, B<C**, B<(D, E, F)***, C<F* |
| 5-year mortality | 94 (14.8) | 213 (18.6) | 448 (26.3) | 528 (31.9) | 315 (31.7) | 179 (42.0) | <0.001 | A<(C, D, E, F)***, B<(C, D, E, F)***, C<D**, C<F***, D<F**, E<F** |
Values are presented as number (%). p-value indicates the result of omnibus test. Group A: Patient’s age of 65-69 years. Group B: Patient’s age of 70-74 years. Group C: Patient’s age of 75-79 years. Group D: Patient’s age of 80-84 years. Group E: Patient’s age of 85-89 years. Group F: Patient’s age of ≥90 years.
Table 2.
| Cluster 1 | Cluster 2 | Cluster 3 | p | Post hoc (Bonferroni) | |
|---|---|---|---|---|---|
| Total | 2,800 (42.7) | 2,900 (44.2) | 856 (13.1) | ||
| Group A | 390 (13.9) | 213 (7.3) | 32 (3.7) | <0.001 | |
| Group B | 582 (20.8) | 473 (16.3) | 90 (10.5) | ||
| Group C | 694 (24.8) | 805 (27.8) | 202 (23.6) | ||
| Group D | 616 (22.0) | 782 (27.0) | 256 (29.9) | ||
| Group E | 377 (13.5) | 458 (15.8) | 160 (18.7) | ||
| Group F | 141 (5.0) | 169 (5.8) | 116 (13.6) | ||
| Age (yr) | 77.8±7.1 | 79.3±6.5 | 81.6±6.8 | ||
| Female | 1,447 (51.7) | 1,640 (56.6) | 383 (44.7) | <0.001 | 1<2*, 1>3*, 2>3* |
| Stroke | 1,319 (47.1) | 2,257 (77.8) | 703 (82.1) | <0.001 | 1<(2, 3)***, 2<3* |
| Bone fracture | 234 (8.4) | 300 (10.3) | 181 (21.1) | <0.001 | 1<2**, 1<3*, 2<3*** |
| Medical history | |||||
| PVD | 97 (3.5) | 329 (11.3) | 68 (7.9) | <0.001 | 1<(2, 3)***, 2>3** |
| COPD | 849 (30.3) | 1,800 (62.1) | 607 (70.9) | <0.001 | 1<(2, 3)***, 2<3*** |
| Cancer | 427 (15.3) | 710 (24.5) | 234 (27.3) | <0.001 | 1<(2, 3)*** |
| Diabetes | 917 (32.8) | 1,855 (64.0) | 477 (55.7) | <0.001 | 1<(2, 3)***, 2>3** |
| Dyslipidemia | 255 (9.1) | 1,573 (54.2) | 384 (44.9) | <0.001 | 1<(2, 3)***, 2>3*** |
| UGI beeding | 47 (1.7) | 113 (3.9) | 129 (15.1) | <0.001 | 1<(2, 3)***, 2<3*** |
| Hypertension | 1,967 (70.3) | 2,827 (97.5) | 809 (94.5) | <0.001 | 1<(2, 3)***, 2>3** |
| Lung infection | 60 (2.1) | 48 (1.7) | 483 (56.4) | <0.001 | 1<3***, 2<3*** |
| Nasogastric tube | 92 (3.3) | 67 (2.3) | 674 (78.7) | <0.001 | 1<3***, 2<3*** |
| Urinary infection | 288 (10.3) | 450 (15.5) | 485 (56.7) | <0.001 | 1<(2, 3)***, 2<3*** |
| Myocardial infarction | 0 (0.0) | 232 (8.0) | 50 (5.8) | <0.001 | 1<(2, 3)*** |
| Chronic kidney disease | 160 (5.7) | 418 (14.4) | 142 (16.6) | <0.001 | 1<2***, 1<3*** |
| Coronary artery disease | 553 (19.8) | 2,625 (90.5) | 542 (63.3) | <0.001 | 1<(2, 3)***, 2>3*** |
| Congestive heart failure | 91 (3.3) | 1,192 (41.1) | 314 (36.7) | <0.001 | 1<(2, 3)*** |
| 5-year mortality | 494 (17.6) | 773 (26.7) | 510 (59.6) | <0.001 | 1<(2, 3)**, 2>3*** |
Values are presented as mean±standard deviation or number (%). Group A: Patient’s age of 65-69 years. Group B: Patient’s age of 70-74 years.
Group C: Patient’s age of 75-79 years. Group D: Patient’s age of 80-84 years. Group E: Patient’s age of 85-89 years. Group F: Patient’s age of ≥90 years. Cluster 1: Low comorbidity class. Cluster 2: Cardiometabolic multimorbidity class. Cluster 3: FRINGED class (characterized by FRacture, Infection, NasoGastric feeding, and bleEDing over upper gastrointestinal tract). p-value indicates the result of omnibus test.
Table 3.
Group A: Patient’s age of 65-69 years. Group B: Patient’s age of 70-74 years. Group C: Patient’s age of 75-79 years. Group D: Patient’s age of 80-84 years. Group E: Patient’s age of 85-89 years. Group F: Patient’s age of ≥90 years. OR, odd ratio; CI, confidence interval; PVD, peripheral vascular disease; COPD, chronic obstructive pulmonary disease; UGI bleeding, upper gastrointestinal bleeding
REFERENCES
- TOOLS







