 |
 |
- Search
| Psychiatry Investig > Volume 20(12); 2023 > Article |
|
Abstract
Objective
Methods
Results
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Seockhoon Chung, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Seockhoon Chung. Data curation: Eulah Cho, Inn-Kyu Cho, Dongin Lee, Jiyoung Kim. Formal analysis: Sohyeong Kim, Seockhoon Chung. Methodology: Eulah Cho, Seockhoon Chung. Writing—original draft: Seockhoon Chung, Sohyeong Kim, Inn-Kyu Cho, Dongin Lee, Jiyoung Kim. Writing—review & editing: all authors.
Funding Statement
This study was supported by the Korea government (MIST) [2021-0-01521, Development of patient-specific cognitive behavioral therapy (CBT-I) digital treatment technology to improve insomnia].
Figure 1.
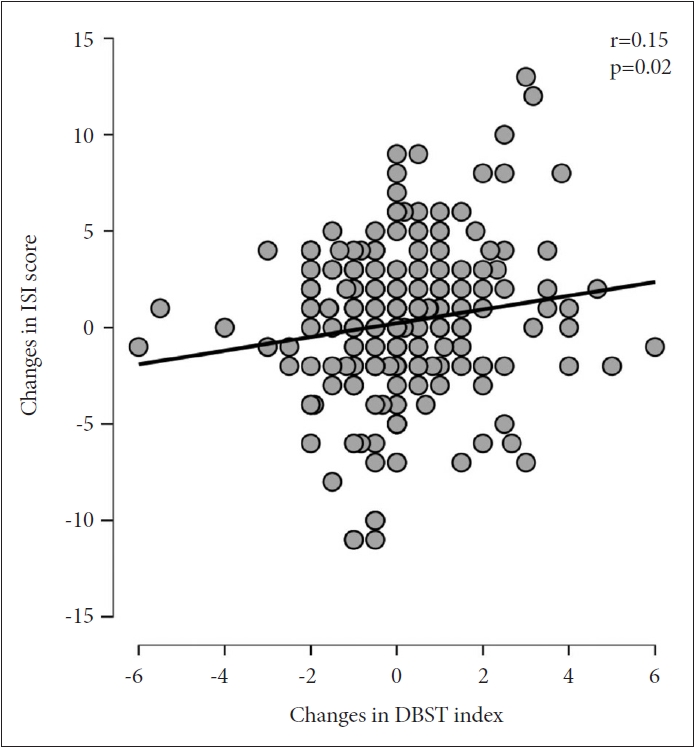
Figure 2.
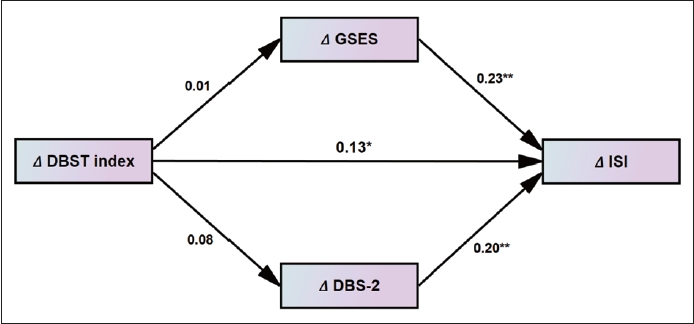
Table 1.
Table 2.
| Variable | Age | ISI | GSES | DBS-2 | dTST | dBT | dWT | dTIB |
|---|---|---|---|---|---|---|---|---|
| At baseline (T1, N=399) | ||||||||
| ISI | -0.03 | |||||||
| GSES | -0.12* | 0.55** | ||||||
| DBS-2 | -0.04 | 0.22** | 0.15** | |||||
| dTST | -0.24** | -0.08 | -0.03 | -0.02 | ||||
| dBT | -0.22** | -0.04 | 0.02 | -0.10* | -0.08 | |||
| dWT | -0.33** | 0.06 | 0.06 | -0.04 | 0.36** | 0.22** | ||
| dTIB | -0.12* | 0.07 | 0.03 | 0.04 | 0.37** | -0.55** | 0.69** | |
| DBST index | -0.06 | 0.14** | 0.05 | 0.05 | -0.40** | -0.48** | 0.41** | 0.70** |
| At follow-up (T2, N=233) | ||||||||
| ISI | -0.01 | |||||||
| GSES | 0.01 | 0.67** | ||||||
| DBS-2 | 0.04 | 0.20** | 0.23** | |||||
| dTST | -0.25** | -0.07 | -0.04 | -0.01 | ||||
| dBT | -0.20** | -0.16* | -0.07 | -0.14* | -0.02 | |||
| dWT | -0.42** | 0.04 | 0.08 | -0.11 | 0.39** | 0.34** | ||
| dTIB | -0.22** | 0.17* | 0.14* | 0.02 | 0.36** | -0.51** | 0.64** | |
| DBST index | -0.01 | 0.22** | 0.16* | 0.02 | -0.51** | -0.45** | 0.26** | 0.61** |
DBST index, discrepancy between desired time in bed and desired total sleep time; ISI, Insomnia Severity Index; GSES, Glasgow Sleep Effort Scale; DBS-2, Dysfunctional Beliefs about Sleep-2 items; dTST, desired total sleep time; dBT, desired bedtime; dWT, desired wake-up time; dTIB; desired time in bed
Table 3.
Table 4.
| Variable | Age | ΔISI | ΔGSES | ΔDBS-2 | ΔdTST | ΔdBT | ΔdWT | ΔdTIB |
|---|---|---|---|---|---|---|---|---|
| ΔISI | -0.03 | |||||||
| ΔGSES | -0.14* | 0.24** | ||||||
| ΔDBS-2 | -0.07 | 0.22** | 0.06 | |||||
| ΔdTST | 0.02 | 0.09 | 0.08 | -0.03 | ||||
| ΔdBT | -0.01 | 0.01 | -0.02 | -0.01 | -0.12 | |||
| ΔdWT | 0.03 | -0.02 | -0.10 | -0.13 | 0.22** | -0.04 | ||
| ΔdTIB | 0.02 | -0.02 | -0.05 | -0.07 | 0.23** | -0.77** | 0.67** | |
| ΔDBST index | 0.05 | 0.15* | 0.01 | -0.08 | -0.50** | -0.51** | 0.32** | 0.58** |
DBST index, discrepancy between desired time in bed and desired total sleep time; ISI, Insomnia Severity Index; GSES, Glasgow Sleep Effort Scale; DBS-2, Dysfunctional Beliefs about Sleep-2 items; dTST, desired total sleep time; dBT, desired bedtime; dWT, desired wake-up time; dTIB; desired time in bed
Table 5.
Table 6.
REFERENCES







