|
 |
- Search
| Psychiatry Investig > Volume 21(5); 2024 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Kyungmin Kim, Jungmin Woo. Data curation: Kyungmin Kim. Methodology: Kyungmin Kim, Jungmin Woo. Formal analysis: Kyungmin Kim, Jungmin Woo. Investigation: Kyungmin Kim, Jungmin Woo. WritingŌĆöoriginal draft: Kyungmin Kim. WritingŌĆöreview & editing: Kyungmin Kim, Jungmin Woo.
Funding Statement
None
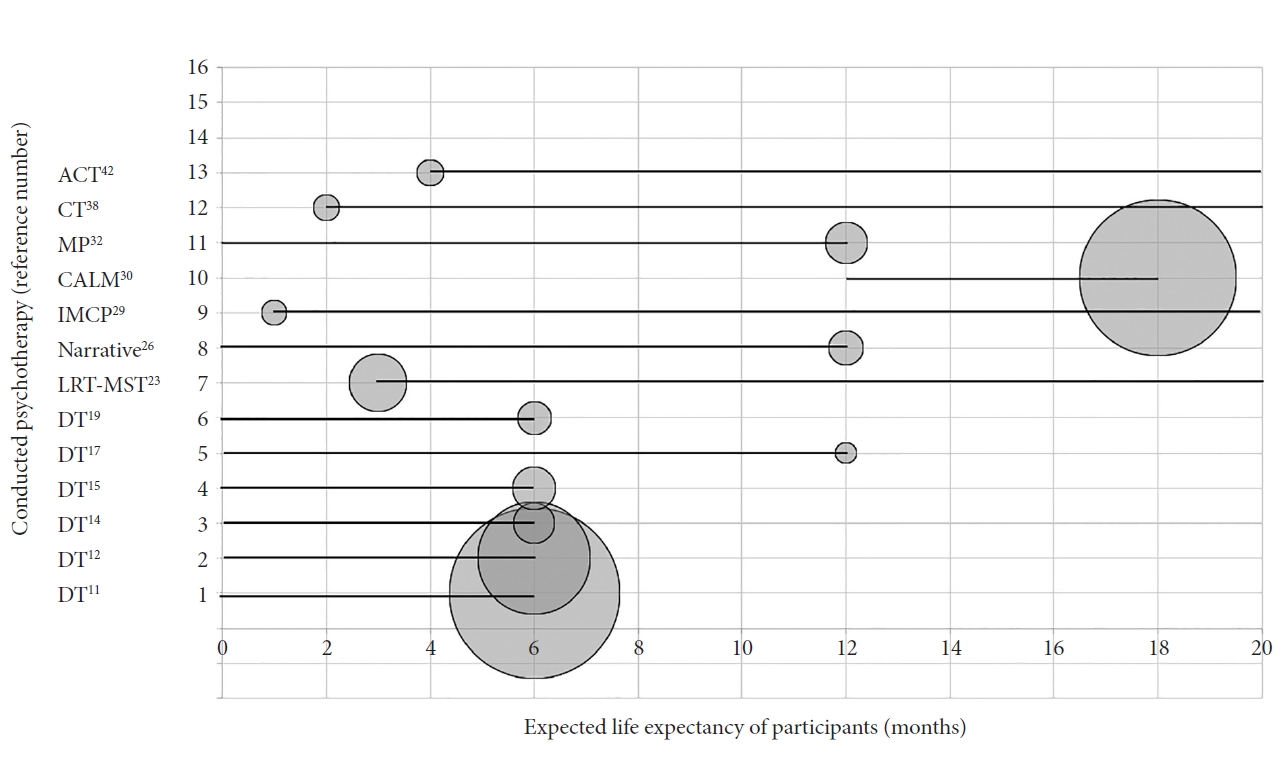
Figure┬Ā2.
Table┬Ā1.
| Author (published year), country | Study period | Participants | Intervention (N) | Control (N) | Outcomes | Measures |
|---|---|---|---|---|---|---|
| Chochinov et al. (2011) [11] Canada, USA, and Australia | April 2005-October 2008 | - 18 years or older individuals | DT (N=165) | Client-centred care (N=140) or SPC (N=136) | - No significant differences in reductions in various dimensions of distress | - Palliative performance scale |
| - Terminal prognosis with expected life expectancy Ōēż6 months | - FACIT | |||||
| - Significant improvement in quality of life, sense of dignity in selfreported end of-life experiences | - Spiritual Well-Being Scale | |||||
| - Receiving palliative care in a hospital or community setting | - PDI | |||||
| - HADS | ||||||
| - No cognitive impairments (hospice or home) | - Structured interview for symptoms and concerns (items including dignity, desire for death, suffering, hopelessness, depression, suicidal idea and sense of burden to others) | |||||
| - Quality of life scale (two-items) | ||||||
| - Modified ESAS | ||||||
| Scarton et al. (2018) [12] Canada, USA, and Australia | April 2005-October 2008 | - 18 years or older individuals | DT (N=108) | Client-centred care (N=107) or SPC (N=111) | - Intervention group showed a higher Dignity impact ratings compared to both other groups | - The 7-item of Dignity Impact Scale |
| - Terminal prognosis with expected life expectancy Ōēż6 months | ||||||
| - Receiving palliative care in a hospital or community setting (hospice or home) | ||||||
| - No cognitive impairments | ||||||
| Hall et al. (2011) [13] UK | April 2009-June 2010 | - No cognitive impairments | DT (N=23) | SPC (N=22) | - No significant differences in dignity related distress | - Primary outcome |
| - Patients with advanced cancer | ŌĆā- PDI (dignity-related distress) | |||||
| - Aged 18 years or more | - Intervention group showed higher levels of hope than the control group with medium effect size | - Secondary outcomes | ||||
| - Referred to hospital based palliative care teams | ŌĆā- Herth Hope Index (hope) | |||||
| - Excluded if the palliative care team felt they were unable to take part in a protocol lasting 2 weeks | - No difference in anxiety, depression, quality of life or palliative outcomes | ŌĆā- HADS (psychological distress) | ||||
| - No cognitive impairments | ŌĆā- EQ-5D (quality of life) | |||||
| ŌĆā- Palliative care outcomes | ||||||
| Juli├Żo et al. (2014) [14] Portugal | May 2010-May 2013 | - Participants with 18 or more years of age | DT (N=39) | SPC (N=41) | - DT had beneficial effect in depression and anxiety, sustained for 30 days follow up period | - HADS; baseline (T1), day 4 (T2), day 15 (T3), day 30 (T4) of follow-up |
| - Having a life-threatening disease with a prognosis of 6 months or less | ||||||
| - Mini Mental State score 20 or more | ||||||
| Juli├Żo et al. (2017) [15] Portugal | May 2010-May 2013 | - Participants with 18 or more years of age | DT (N=41) | SPC (N=39) | - DT was associated with significant decrease in DS and desire for death | - DS |
| - Having a life-threatening disease with a prognosis of 6 months or less | - DT participants showed significant decrease in 19 of 25 PDI questions (except cognitive capacity, meaningful life and healthcare support) | - Desire for Death Rating Scale | ||||
| - Mini Mental State score 20 or more | - PDI | |||||
| Rudilla et al. (2016) [16] Spain | April 2013-June 2013 | - 18 years or older patients | DT (N=35) | Counselling therapy (N=35) | - Both DT and counseling group showed positive effect on perception of meaning in life, quality of life and spiritual well-being | - PDI |
| - From a palliative care, home care unit with advanced/terminal illness | - HADS | |||||
| - Brief Resilient Coping Scale | ||||||
| - Less than 2 weeks of predicted survival were excluded | - Significantly higher effect on anxiety in counseling group | - GES Questionnaire; Spirituality | ||||
| - No cognitive impairments | - Duke-UNC-11 Functional Social Support Questionnaire | |||||
| - No other significant differences were found in outcomes comparing two groups | - Two items from the EORTC Quality of Life C30 Questionnaire (EORTC-QLQ-C30) | |||||
| ŌĆā- ŌĆ£ How would you rate your overall health during the past week?ŌĆØ | ||||||
| ŌĆā- ŌĆ£ How would you rate your overall quality of life during the past week?ŌĆØ | ||||||
| Vuksanovic et al. (2017) [17] Australia | March 2012-December 2015 | - 18 years or older individuals | DT (N=20) | LR (N=18) | - DT significantly improved generativity and ego integrity | - Brief Generativity and Ego-Integrity |
| - Advanced disease with a life expectancy of less than 12 months based on clinical consensus | WC (N=18) | - No group differences for dignity related distress or physical, social, emotional and functional well-being among three groups | - PDI | |||
| - Receiving specialist multidisciplinary palliative care either in a hospital or home setting | - FACT-G, version 4: QOL | |||||
| - No cognitive impairments | - A treatment evaluation form | |||||
| Weru et al. (2020) [18] Kenya | August 2016-March 2017 | - Adults aged between 18 and 65 years | DT (N=72) | UC (N=72) | - No statistical effect on overall quality of life score, but improvement in summated symptom score in DT group compared to the control group | - ESAS: quality of life |
| - Advanced cancers (stage 3 and 4) | ||||||
| - Recruited from the inpatient hospital setting and outpatient oncology clinics | ||||||
| - No cognitive impairments | - Anxiety symptom score showed a trend toward significance (p=0.059) | |||||
| Iani et al. (2020) [19] Italy | February 2018-May 2020 from | - Age over 18 | DT (N=32) | SPC (N=32) | - Unlike control group, DT reported the effect of protecting the decline of peace | - Primary outcomes |
| - Diagnosis of life-threatening disease with a prognosis ranging from 1 to 6 months (based on the evaluation of physicians who referred patients) | ŌĆā- FACIT-Spiritual Well-Being Scale (FACIT-Sp) | |||||
| - No significant longitudinal changes measured of meaning, faith, loss of MaP, coping ability and distress | - 2ndary outcome | |||||
| - No cognitive impairments | ŌĆā- DS-II | |||||
| ŌĆā- PDI (dignity related distress) | ||||||
| Ando et al. (2010) [20] Japan | April 2007-March 2008 | - Terminally ill patients with incurable cancer | Short-term LR interview (N=38) | General support (N=39) | - Short-term LR reported effectiveness in improving the spiritual well-being, hope, life completion and preparation than control group | - Primary outcomes |
| - Over age 20 years | ŌĆā- FACIT-Sp scale; meaning of life domain | |||||
| - Undergoing treatment in the PCU; duration in the PCU was between two and four weeks | - Intervention showed decreased depression, anxiety, burden and suffering compared to control group | - Secondary outcomes | ||||
| ŌĆā- HADS | ||||||
| - No cognitive impairments | ŌĆā- Good Death Inventory (hope, burden, life completion, and preparation) | |||||
| ŌĆā- A numeric scale for psychological suffering | ||||||
| Xiao et al. (2013) [22] China | Not mentioned | - Patients with advanced cancer | LRT (N=40) | Routine care through home visits and weekly telephone follow-up (N=40) | - In the intervention group, significantly better outcomes were shown in overall quality of life, support and value of life | - Overall QOL; single-item |
| - Aged 18 years or more | - Quality-of-life concerns: 28-item quality of life concerns in the end-of-life questionnaire | |||||
| - From a home-based hospice | - Reduction in negative emotions, sense of alienation, existential distress were found compared to control group | ŌĆā- 8 subscales: physical discomfort, food-related concerns, healthcare concerns, support, negative emotions, sense of alienation, existential distress, and value of life | ||||
| - Karnofsky Performance Status more than 40 | ||||||
| - No cognitive impairment | ||||||
| Kleijn et al. (2018) [23] Netherlands | June 2010-December 2013 | - Adults over 19 years old | LRT and memory specificity training (N=55) | WC (N=52) | - Ego-integrity improved over time in the intervention group compared to control group | - Primary outcome |
| - All types of cancer receiving palliative care | ŌĆā- Ego-integrity and despair | |||||
| - Expected prognosis more than 3 months | - No significant difference in despair, psychological distress or quality of life | - Secondary outcome | ||||
| - No psychotic behavior or severe cognitive dysfunction | ŌĆā- HADS (psychological distress, anxiety and depression) | |||||
| ŌĆā- The European Organisation for Research and Treatment of Cancer Quality-of-Life Questionnaire PAL 15 (EORTC QLQ-C15-PAL; quality of life) | ||||||
| ŌĆā- Autobiographical Memory Test (specificity of the autobiographical memory) | ||||||
| Wise et al. (2018) [25] USA | Not mentioned | - Age 30 or older patients | miLivingStory; a telephone-based LR and illness narrative intervention (N=49) | miOwnResources; an active control group website with information and support but no story tips (N=37) | - miLivingStory group had a positive effect for peace, and trend effect for lower depressed mood at four months follow up compared to control group | - FACIT-Sp; peace and meaning |
| - Stage III or IV cancer | - Profile of Mood States-Short Form; depressed, angry, and anxious moods | |||||
| - Willingness to use internetenabled computer | - Protection against control groupŌĆÖs declining wellbeing between two and four months follow up were shown | |||||
| Lloyd-Williams et al. (2018) [26] UK | May 2013-December 2015 | - Age older than 18 | Narrative intervention (N=33) | UC (N=24) | - Intervention group had greater reduction in PHQ-9 score at 6-week follow-up (p=0.04) | - PHQ-9 |
| - Advanced cancer patients attending hospice day care services | - ESAS; pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being and shortness of breath | |||||
| - Eastern Cooperative Oncology Group one or two | - Median survival was longer (157 days) for intervention and compared to control group (102 days, p=0.07) | |||||
| - Life expectancy of 12 months or less | ||||||
| - No severe cognitive impairment | ||||||
| - Exclude prognosis of 6 weeks or less | ||||||
| - All participants were depression cases at baseline (PHQ-9Ōēź10) | ||||||
| Breitbart et al. (2018) [28] USA | March 2011-March 2016 | - Patients age 18 years or more | IMCP (N=109) | Supportive psychotherapy (N=108) or EUC | - Significant treatment effects (small to medium in magnitude) were observed for IMCP, in comparison with EUC, in quality of life, sense of meaning, spiritual well-being, anxiety, and desire for hastened death | - Primary outcomes; existential distress and overall quality of life |
| - Have a stage IV solid tumor cancer | ŌĆā- FACIT-Sp Well-Being Scale | |||||
| - Have at least moderate distress (DT score of 4 or higher) | ŌĆā- Personal Meaning Index of the Life Attitude Profile-Revised | |||||
| - No severe cognitive impairment or psychiatric disturbance (psychosis or suicidal ideation) | - No significant improvement was observed for patients receiving SP | ŌĆā- MQOL | ||||
| - Secondary outcomes; psychological distress | ||||||
| - The effect of IMCP was significantly greater than the effect of SP for quality of life and sense of meaning but not for the remaining study variables | ŌĆā- Hopelessness Assessment in Illness questionnaire | |||||
| ŌĆā- Schedule of Attitudes Toward Hastened Death | ||||||
| ŌĆā- HADS | ||||||
| Fraguell-Hernando et al. (2020) [29] Spain | May 2017-April 2018 | - Age 18 years or more | IMCP (N=24) | Counselling (N=27) | - Demoralization (despair), anxiety, depression, and emotional distress were reduced in intervention group | - HADS |
| - Patients with advanced-stage cancer receiving palliative care at home | - Detection of Emotional Distress | |||||
| - Physician estimated life expectancy more than 1 month | - Demoralization was the only variable that significantly improved in the counselling group | - DS-II | ||||
| - No psychiatric disturbance | ||||||
| Rodin et al. (2018) [30] Canada | February 2012-March 2016 | - Age 18 years or more patients | CALM (N=151) | UC (N=154) | - Intervention group showed less-severe depression at 3 and 6 months follow up period | - Primary outcome; PHQ-9 |
| - Diagnosis of stage III or IV lung cancer, any-stage pancreatic cancer, unresectable cholangiocarcinoma, unresectable liver cancer, unresectable ampullary or peri-ampullary cancer or other stage IV gastrointestinal cancer, stage III or IV ovarian and fallopian tube cancers or other stage IV gynecologic cancer, stage IV breast cancer, genitourinary cancer, sarcoma, melanoma, or endocrine cancer | - Secondary outcomes | |||||
| - Better end of life preparation at 6 months follow up period compared to UC group | ŌĆā- GAD-7 | |||||
| ŌĆā- DADDS | ||||||
| ŌĆā- FACIT-Sp Well-Being Scale (FACIT-Sp-12) | ||||||
| ŌĆā- QUAL-EC Scale | ||||||
| - With an expected prognosis of 12 to 18 months | ŌĆā- 16-Item Experiences in Close Relationships Scale validated for use in advanced cancer (ECR-M16) | |||||
| - Excluded cognitive impairment basis of SOMC score less than 20, current psychiatric or psychological treatment | ŌĆā- CCS | |||||
| ŌĆā- PTGI | ||||||
| ŌĆā- DS | ||||||
| Mehnert et al. (2020) [31] Germany | August 2013-January 2017 | - Age 18 years or more | CALM (N=99) | Non-manualized supportive psychooncological counselling intervention (SPI) (N=107) | - Significantly less depressive symptoms at 6 months than at baseline but no group differences in depression severity | - Primary outcome: depression |
| - Had a malignant solid tumor; Union for International Cancer Control III or IV stages | ŌĆā- BDI-revision (BDI-II) | |||||
| ŌĆā- PHQ-9 | ||||||
| - Score of Ōēź9 on the PHQ-9, and/or Ōēź5 on the distress thermometer | - No significant group differences on secondary outcomes either | - Secondary outcomes | ||||
| ŌĆā- Psychological distress; distress thermometer | ||||||
| - Excluded | ŌĆā- Quality of life; QUAL-EC | |||||
| - Severe cognitive impairment (Ōēż20 on SOMC) | ŌĆā- Anxiety; GAD-7 Questionnaire | |||||
| - High level of functional impairments (Karnofsky score Ōēż70) | ŌĆā- Demoralization; DS | |||||
| ŌĆā- Fatigue; Brief Fatigue Inventory | ||||||
| - If they reported suicidal ideation | ŌĆā- Symptom burden; Memorial Symptom Assessment Scale (MSAS-SF29) | |||||
| - If they reported suicidal ideation | ŌĆā- Spiritual well-being; Functional Assessment of Chronic | |||||
| ŌĆā- Illness Therapy Spiritual Well-Being Scale (FACIT-Sp) | ||||||
| ŌĆā- Death anxiety DADDS | ||||||
| ŌĆā- Posttraumatic growth; PTGI | ||||||
| ŌĆā- Attachment insecurity; Experiences in Close Relationships Scale (ECR-M16) | ||||||
| ŌĆā- Couple communication; CCS | ||||||
| Kissane et al. (2019) [32] Australia | 2015-2016 | - Age >18 years | MaP therapy (N=40) | Wait list UC (N=17) | - MaP therapy showed effectiveness in posttraumatic growth (new possibilities, appreciation of life, and personal strength) and life attitudes (choices and goal seeking) compared to control group | - PTGI |
| - Advanced cancer | - The Life Attitude Profile-Revised | |||||
| - Whose prognosis was assessed at 12 months or less | - Brief Symptom Inventory | |||||
| - No cognitive or psychiatric impairments | - DS-II | |||||
| - Existential distress: FACIT-Sp-12 meaning subscale | ||||||
| - MQOLexistential subscale | ||||||
| Henry et al. (2010) [35] Canada | Not mentioned | - Age 18 years or older | Meaning making interventioin (N=12) | UC (N=12) | - Intervention group had a better sense of meaning in life at one and three months post-intervention | - HADS |
| - Stage III or IV ovarian cancer patients | - General Self-Efficacy Scale; perception of his or her general ability to deal with new or difficult situations | |||||
| - Diagnosed within the last two months | - No significant effectiveness in anxiety, depression and self-efficacy compared to control group | |||||
| - Physically and emotionally capable participating without burden (ECOG performance status 1 or 2) | ||||||
| Mok et al. (2012) [36] Hong Kong | September 2010-March 2011 | - 18 years or older aged | Meaning of life intervention (N=44) | UC (N=40) | - Intervention group showed significant effects in the QOLC-E total score, and existential distress subscale. Single item scale on global quality of life also showed improvement | - Quality-of-Life Concerns in the End-of-Life (QOLC-E) questionnaire |
| - Diagnosed advanced-stage cancer (refractory to established curative treatments or for which no established curative treatments existed) | - Single-item scale on global quality of life | |||||
| - Recruited from oncology inpatient ward | ||||||
| - Excluded if they had significant cognitive impairment or psychoses | ||||||
| Savard et al. (2006) [38] Canada | May 1999-June 2003 | - Women who diagnosed in metastatic breast cancer (stage IV) | Cognitive therapy for advanced cancer (N=25) | WC (N=20) | - Significant lowering in depression using HDRS | - HADS |
| - 7 or more on the HADS-D or of 15 or more on the BDI Score | - Were found in intervention group compared to control | - BDI | ||||
| - Excluded criteria | - Using a pooled data set, a significant effect in lower the symptoms including depression, anxiety, fatigue and insomnia were found | - HDRS | ||||
| - Life expectancy less than 2 months | - Insomnia Severity Index | |||||
| - Patients with DSM-IV criteria severe psychiatric disorder other than major depression | - Multidimensional Fatigue Inventory | |||||
| - Recent antidepressant start (with in 2 month) | - No treatment effect was found on any of the immune variables | - The European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ-C33) | ||||
| - Suicidal ideation/acting out using Scale for Suicide Ideation | - EORTC Breast Cancer-Specific Quality of Life Questionnaire Module (QLQ-BR23) | |||||
| - Currently receiving a psychological intervention for depression | - Health Behaviors Questionnaire | |||||
| - List of life events | ||||||
| - Secondary outcome: immune function | ||||||
| Moorey et al. (2009) [39] UK | March 2004-December 2005 | - Patients with palliative home care | CBT, for palliative care (N=45) | TAU (N=35) | - Individuals receiving CBT had lower anxiety scores over time | - HADS |
| - Who score 8 or more for anxiety or depression on the HADS on either subscale | - The Mental Adjustment to Cancer Scale | |||||
| - Excluded significant cognitive, communication difficulties | - No significant effect was shown in depression | - The Cancer Coping Questionnaire measure the coping strategies taught in CBT for cancer | ||||
| - The Multi-dimensional Scale of Perceived Social Support 12-item self-report measure of perceived social support | ||||||
| - The Eastern Cooperative Oncology Group Performance Status Scale | ||||||
| Greer et al. (2012) [40] USA | October 2007-June 2010 | - Age 18 or more patients | CBT (brief, 6 session or less) (N=20) | WC (N=20) | - Significant reduction in anxiety symptoms compared to control group | - HAM-A |
| - With incurable solid tumor | - Clinical Global Impression Scale | |||||
| - The presence of clinically significant anxiety symptoms (HAM-A score 14 or more), at least 4 weeks after cancer diagnosis | - No significant effects in depressive symptoms | - Montgomery Asberg Depression Rating Scale | ||||
| - HADS | ||||||
| - Impact of Events Scale | ||||||
| - FACT-G Questionnaire; quality of life | ||||||
| Serfaty et al. (2019) [41] UK | Not mentioned | - Patients with advanced cancer and depression (a diagnosis of cancer not amenable to cure, a DSM-IV diagnosis of depressive disorder using the Mini-International Neuropsychiatric Interview) | CBT (N=93) | TAU (N=92) | - CBT showed no significant clinical benefit in advanced cancer patients with depression | - Primary outcome: BDI-II |
| - Secondary outcomes | ||||||
| - A subgroup analysis of those widowed, divorced or separated showed a significant effect of CBT on the BDI-II | ŌĆā- PHQ-9 | |||||
| - Excluded Clinician-estimated survival of <4 months, high suicide examined using the MINI, currently receiving or having received in the last 2 months, a psychological intervention | ŌĆā- Eastern Cooperative Oncology Group Performance Status satisfaction with care | |||||
| ŌĆā- EuroQol-5 Dimensions | ||||||
| ŌĆā- Client Services Receipt Inventory | ||||||
| Rost et al. (2012) [42] USA | Not mentioned | - Women with late-stage ovarian cancer (stage III or IV) | ACT (CBT) (N=25) | TAU (N=22) | - Significant effect improving quality of life, reduction in psychological distress in intervention group | - BDI-II |
| - Beck Anxiety Inventory | ||||||
| - Profile of Mood States: distress | ||||||
| - No significant effect on anxiety or depressive symptoms compared to control group | - Courtland Emotional Control Scale: emotional control | |||||
| - White Bear Thought Suppression Inventory thought suppression inventory | ||||||
| - COPE: assesses general strategies of coping | ||||||
| - FACT-G: QOL |
SPC, standard palliative care; FACIT, Functional Assessment of Chronic Illness Therapy; PDI, Patient Dignity Inventory; HADS, Hospital Anxiety and Depression Scale; ESAS, Edmonton Symptom Assessment Scale; DS, demoralization syndrome; LR, life-review; WC, waitlist control; UC, usual care; MaP, meaning and purpose; LRT, life review therapy; PHQ, Patient Health Questionnaire-9; EUC, enhanced usual care; MQOL, McGill Quality of Life Questionnaire; DS-II, Short Demoralization Scale; GAD-7, Generalized Anxiety Disorder-7; DADDS, Death and Dying Distress Scale; QUAL-EC, Quality of Life at the End of Life Cancer Scale; CCS, Couple Communication Scale; PTGI, Posttraumatic Growth Inventory; DS, Demoralization Scale; DT, dignity therapy; SOMC, Short Orientation-Memory-Concentration Test; BDI, Beck-Depressions-Inventory; TAU, treatment as usual; HDRS, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale; FACT-G, Functional Assessment of Cancer Therapy-General; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; PCU, palliative care unit; IMCP, individual meaning-centered psychotherapy; CALM, cancer and living meaningfully; SP, supportive psychotherapy
REFERENCES