 |
 |
- Search
| Psychiatry Investig > Volume 21(5); 2024 > Article |
|
Abstract
Objective
Methods
Results
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Seockhoon Chung, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Marta Moraleda-Cibri├Īn. Data curation: Marta Moraleda-Cibri├Īn. Formal analysis: Marta Moraleda-Cibri├Īn. Funding acquisition: Marta Moraleda-Cibri├Īn. Investigation: Marta Moraleda-Cibri├Īn. Methodology: Marta Moraleda-Cibri├Īn. Project administration: Marta Moraleda-Cibri├Īn. Resources: Marta Moraleda-Cibri├Īn. Supervision: Seockhoon Chung. WritingŌĆöoriginal draft: Marta Moraleda-Cibri├Īn. WritingŌĆöreview & editing: all authors.
Funding Statement
This study was supported by the Spanish Sleep Society (SES Research Award 2020).
ACKNOWLEDGEMENTS
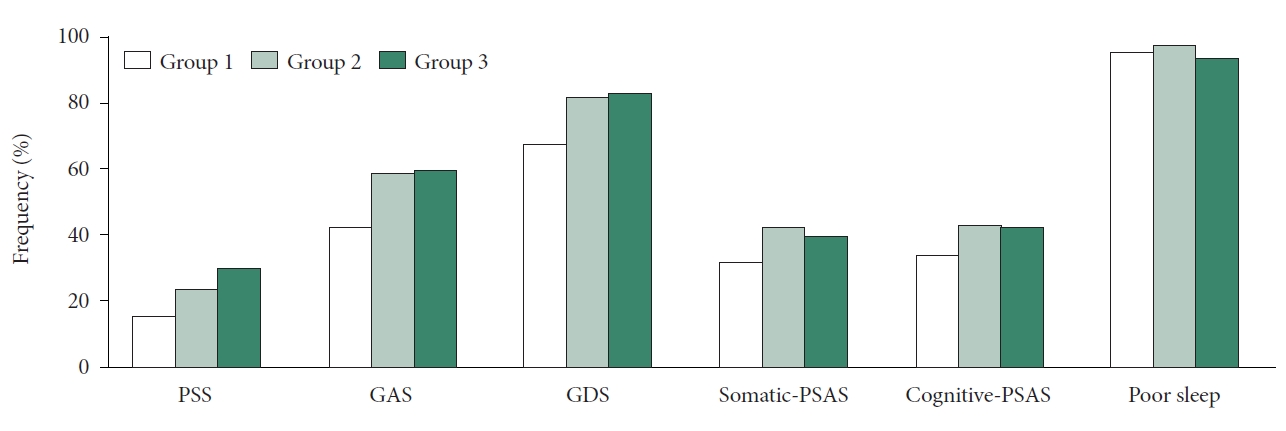
Figure┬Ā2.
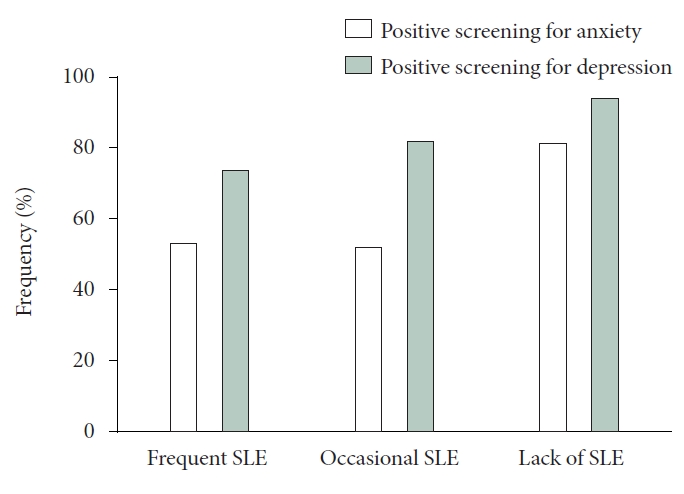
Figure┬Ā3.
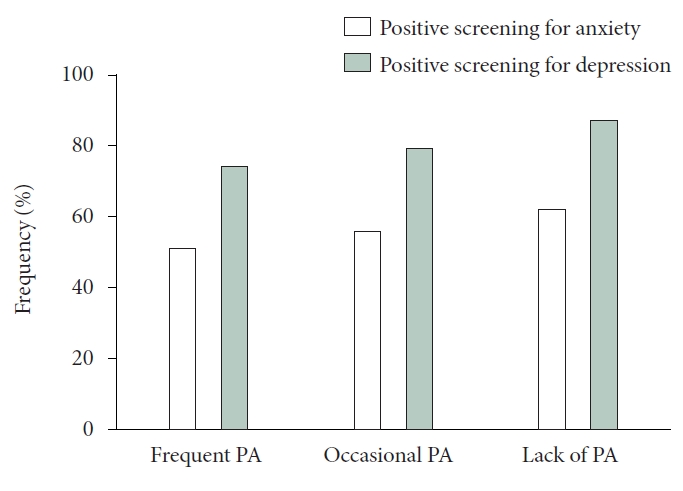
Figure┬Ā4.
Table┬Ā1.
Table┬Ā2.
| Severe stress (PSS) | Positive anxiety (GAS) | Positive depression (GDS) | Somatic symptoms (PSAS) | Cognitive symptoms (PSAS) | Poor sleeper (PSQI) | |
|---|---|---|---|---|---|---|
| Age (yr) | ||||||
| ŌĆā25.0-34.9 | 25┬▒19.2 | 80┬▒61.6* | 116┬▒89.2** | 71┬▒54.6** | 53┬▒40.8 | 127┬▒97.7 |
| ŌĆā35.0-49.9 | 70┬▒24.3 | 165┬▒57.3 | 221┬▒76.7 | 95┬▒33.0 | 121┬▒42.0 | 278┬▒96.5 |
| ŌĆā>50 | 36┬▒24.8 | 65┬▒44.8 | 106┬▒73.1 | 56┬▒38.6 | 56┬▒38.6 | 139┬▒95.9 |
| Sex | ||||||
| ŌĆāMale | 12 (11.5) | 41 (39.4) | 70 (67.3) | 29 (27.9) | 40 (38.5) | 96 (92.3) |
| ŌĆāFemale | 119 (25.9)** | 269 (58.6)** | 373 (81.3)** | 193 (42.0)** | 190 (41.4) | 48 (96.7)** |
| Living situation | ||||||
| ŌĆāWith partner | 100 (23.6) | 223 (52.6) | 330 (77.8) | 158 (37.3) | 168 (39.6) | 407 (96.0) |
| ŌĆāSingles | 31 (22.3) | 87 (62.6)* | 113 (81.3) | 64 (46.0) | 62 (44.6) | 137 (98.6) |
| ŌĆāWith dependents | 85 (24.1) | 186 (52.7) | 267 (75.6) | 124 (35.1) | 139 (39.4) | 340 (96.3) |
| ŌĆāWithout dependents | 46 (21.9) | 124 (59.0) | 176 (83.8)* | 98 (46.7)** | 91 (43.3) | 204 (97.1) |
| Professional information | ||||||
| ŌĆāPhysicians | 78 (18.4) | 224 (53.0) | 322 (76.1) | 142 (33.6) | 161 (38.1) | 409 (96.7) |
| ŌĆāNurses | 53 (37.8)** | 86 (61.4) | 121 (86.4)* | 80 (57.1)** | 69 (49.3)* | 135 (96.4) |
| ŌĆāPlace of work | ||||||
| ŌĆāŌĆāHospital | 113 (24.4) | 261 (56.2) | 375 (80.8)* | 188 (40.5) | 197 (42.5) | 451 (97.2) |
| ŌĆāŌĆāPrimary care center | 13 (15.9) | 40 (48.8) | 56 (68.3) | 26 (31.7) | 27 (32.9) | 78 (95.1) |
| ŌĆāŌĆāOthers (geriatric center, COVID-19 center, others) | 5 (29.4)* | 9 (52.9) | 12 (70.6) | 8 (47.1) | 6 (35.3) | 15 (88.2) |
| ŌĆāJob position | ||||||
| ŌĆāŌĆāConsultant/coordinator | 75 (19.4) | 206 (53.2) | 290 (74.9) | 127 (32.8) | 148 (38.2) | 371 (95.9) |
| ŌĆāŌĆāClinical training/others | 56 (31.8)** | 104 (59.1) | 153 (86.9)** | 95 (54.0)** | 82 (46.6) | 173 (98.3) |
| COVID-19 infection | ||||||
| ŌĆāYes | 37 (37.4)** | 67 (67.7)** | 89 (89.9)** | 49 (49.5)* | 54 (54.4)** | 97 (98.0) |
| ŌĆāNo | 94 (20.3) | 243 (52.4) | 354 (76.3) | 173 (37.3) | 176 (37.9) | 447 (96.3) |
Table┬Ā3.
| All the population (N=563) |
Group 1 |
Group 2 |
p* |
Group 3 |
p** | |
|---|---|---|---|---|---|---|
| Baseline, healthcare workers of non-COVID-19 patients (N=145) | Baseline, healthcare workers of COVID-19 patients (N=280) | Follow-up, healthcare workers of COVID-19 patients (N=138) | ||||
| PSS | ||||||
| ŌĆāMean┬▒SD | 23.2┬▒4.6 | 22.2┬▒4.8 | 23.6┬▒4.3 | 23.4┬▒4.7 | ||
| ŌĆāSevere | 131 (23.3) | 23 (15.9) | 66 (23.6) | 0.143 | 42 (30.4) | 0.317 |
| GAS | ||||||
| ŌĆāPositive screening | 310 (55.1) | 62 (42.8) | 165 (58.9) | 0.002 | 83 (60.1) | 0.812 |
| GDS | ||||||
| ŌĆāPositive screening | 443 (78.7) | 98 (67.6) | 230 (82.1) | 0.001 | 115 (83.3) | 0.763 |
| PSAS | ||||||
| ŌĆāSomatic PSAS | 13.2┬▒4.7 | 12.4┬▒4.5 | 13.6┬▒4.6 | 13.6┬▒4.8 | ||
| ŌĆāPositive screening | 222 (39.4) | 47 (32.4) | 120 (42.9) | 0.037 | 55 (39.9) | 0.559 |
| ŌĆāCognitive PSAS | 18.5┬▒6.6 | 17.5┬▒6.5 | 19.1┬▒6.5 | 18.5┬▒6.9 | ||
| ŌĆāPositive screening | 230 (40.9) | 50 (34.5) | 121 (43.2) | 0.082 | 59 (42.8) | 0.929 |
| PSQI | ||||||
| ŌĆāComponent 1 | 1.8┬▒1.3 | 1.6┬▒1.3 | 1.9┬▒1.2 | 1.8┬▒1.3 | ||
| ŌĆāComponent 2 | 1.5┬▒0.8 | 1.3┬▒0.8 | 1.7┬▒0.8 | 1.3┬▒0.8 | ||
| ŌĆāComponent 3 | 1.8┬▒0.8 | 1.7┬▒0.8 | 1.8┬▒0.8 | 1.7┬▒0.8 | ||
| ŌĆāComponent 4 | 2.6┬▒1.0 | 2.8┬▒0.7 | 2.6┬▒1.1 | 2.6┬▒1.0 | ||
| ŌĆāComponent 5 | 1.3┬▒0.5 | 1.2┬▒0.5 | 1.3┬▒0.6 | 1.3┬▒0.6 | ||
| ŌĆāComponent 6 | 0.8┬▒1.1 | 0.7┬▒1.1 | 0.8┬▒1.1 | 0.9┬▒1.2 | ||
| ŌĆāComponent 7 | 1.2┬▒0.8 | 1.1┬▒0.8 | 1.2┬▒0.8 | 1.1┬▒0.8 | ||
| ŌĆāGlobal score | 11.0┬▒3.7 | 10.4┬▒3.9 | 11.3┬▒3.6 | 10.9┬▒3.9 | ||
| ŌĆāPoor sleep | 544 (96.6) | 139 (95.9) | 275 (98.2) | 0.148 | 130 (94.2) | 0.026 |
REFERENCES








