Stress, Mental Health, Sleep, and Healthy Habits in Spanish Healthcare Professionals Along the Pandemic: A Case-Control, and Follow-Up Study
Article information
Abstract
Objective
The aim of this study was to assess short and medium-term impact of the coronavirus disease-2019 (COVID-19) pandemic on stress, mental health, and sleep in Spanish healthcare professionals (HCP), and analyze the association between healthy habits, anxiety, and depression during the same period.
Methods
An online survey including five validated scales (the Perceived Stress Scale, the Goldberg Anxiety and Depression Scales, the Pre-Sleep Arousal Scale, and the Pittsburgh Sleep Quality Index), and some questions about healthy habits were completed by HCP in charge of patients without and with coronavirus. Once for the control group (baseline), and twice for the case group (baseline and follow-up).
Results
Overall 563 questionnaires were included. Moderate-severe stress was reported by 98.1% of subjects, anxiety and depression by 55.1% and 78.7% respectively, and poor sleep quality by 96.6%. Anxiety was reported more frequently by females and singles. HCP in charge of COVID-19 patients showed, in the baseline, a higher frequency of anxiety compared to controls (58.9% vs. 42.8%, p=0.002), and of depression (82.1% vs. 67.6%, p=0.001), that persisted in the follow-up assessment. Furthermore, HCP in charge of COVID-19 patients also exhibited more elevated mean scores for stress (p=0.005) and poor sleep (p=0.019). A decrease of sunlight exposure was associated with an increase of anxiety and depression symptoms, and less physical activity with depression.
Conclusion
Stress, sleep, and mental problems were common in Spanish HCP, especially in those in charge of COVID patients. These findings persisted throughout the pandemic, and may impact in the post-pandemic mental health of HCP.
INTRODUCTION
Stress is a physiological state of organisms that occurs in response to an internal or an external stimulus that challenges or threatens its homeostasis [1,2]. Certain degree of stress is optimal to be alert and to improve adaptability skills. However, when the level of stress exceeds capacity of individuals has a negative impact on daily life, and comorbidities such psychiatric disorders, insomnia, cardiovascular disease, and obesity can appear [3-5]. Causes of stress can be multifactorial. Nevertheless, in the last decades several studies warn about the increase of work-related stress in industrialized societies [6,7].
Before of the pandemic the frequency of psychiatric disorders, and insomnia in Spain was high in adult population. According to survey data of World Health Organization from 2015, 4.1% of the Spanish population had anxiety-related disorders, and 5.2% depression, compared to 3.6%, and 4.4% worldwide data respectively [8]. Moreover, the prevalence of insomnia reached 21% before 2020 [9,10]. However, despite the elevated incidence of psychiatric and sleep disorders in the Spanish population, and the high risk for work-related stress of specific occupations, such as healthcare professionals (HCP), to our knowledge, only few studies, focused mainly on nurses [11,12], have investigated the frequency and the impact of stress in Spanish HCP previously to the pandemic.
The first case of coronavirus disease-2019 (COVID-19) in Spain was diagnosed the 31st of January of 2020 [13]. This viral disease, originated in the Chinese region of Wuhan [14], was characterized by a severe acute respiratory syndrome associated with a high morbidity and mortality, and led in few weeks to the collapse of well-established health systems around the world. The high incidence of COVID-19 in Spain increased the percentage of infections among Spanish health professionals [15], and elevated rates of work-related stress, and mental health symptoms were reported during the first wave of the COVID-19 pandemic [16]. Nevertheless, little is known about the distress, and psychological effects in Spanish HCP who took care of patients with COVID-19 after the outbreak [17]. Therefore, the aims of the present study were: 1) to assess short-term, and medium-term stress, mental health, and sleep quality in Spanish HCP in charge of COVID patients’ overtime compared to HCP in charge of patients with other pathologies, and 2) to investigate the impact of healthy habits in mental health in the study population during the pandemic.
METHODS
Procedure and study population
Participants completed an anonymous online questionnaire that it took between 20 and 30 minutes. The survey was distributed via social media platforms to increase sample size throughout the Spanish geography, and to improve cost-effectiveness. An e-informed consent was obtained before participation in the study, and subjects did not obtain any monetary compensation for participating. Inclusion criteria were as follow: 1) active health personnel during the pandemic (nurses and physicians), 2) aged between 25.0 and 69.9 years, 3) to be in charge of outpatient or admitted patients with and without coronavirus. Study aims were not described in detail to avoid bias survey responses. The study population was divided into two groups: the control and the case group. The control group, HCP in charge of patients without coronavirus, was evaluated once (from April 30th, 2020 to July 1st, 2020). While the case group, HCP in charge of COVID-19 patients, were assessed twice: the baseline assessment, at the begining of the pandemic, as the control group, and the follow-up, at least 6 months later after the first evaluation. It was estimated that the sample size to demonstrate statistically significant differences of 15% of the main variables between the case and the control group with an alpha value of 0.05 and a power of 0.90 was 216. The study was conducted in accordance with the World Medical Association Declaration of Helsinki (seventh revision, Fortaleza 2013), and complies with the guidelines for Good Clinical Research Practices, and the Biomedical Research Law 14/2007. This study was approved by the Ethics Committee of Quirónsalud-Catalonia (2020/52-MSUTEK). Recruitment process has been summarized in Figure 1.
Measurements
The self-administrated survey included three sections. The first section collected general and socio-demographic information such as age, sex, personal (marital status) and professional information (clinical role, medical setting, job category, work schedule (8 hours, 12 hours, 24 hours), and rest schedule per week (1 day, 2 days, >2 days). The second section included five validated scales to investigated stress, mental health (anxiety and depression), hyperarousability state, and quality of sleep.
Perceived Stress Scale
The Perceived Stress Scale (PSS) is an easy tool to assess stress perception in relation to feelings and thoughts experienced in the last month that includes ten questions with five answer options [18]. The score range is between 0–40 and allows to divide the study population into three groups, based on the degree of stress: low (0–13), moderate (14–26), and severe (27–40).
Goldberg Anxiety, and Depression Scales
The Goldberg Anxiety, and Depression Scales (GAS and GDS) were designed for the diagnosis of common psychopathological disorders in primary care such as anxiety, and depression [19]. Each scale includes two parts with nine queries. Positive screening for anxiety was considered when four or more answers were positive (three at least in the first part), and for depression when two or more were positive (one at least in the first part). The Spanish version has demonstrated a sensitivity of 83.1%, a specificity of 81.8%, and a positive predictive value of 95.3%.
Pre-Sleep Arousal Scale
The Pre-Sleep Arousal Scale (PSAS) includes 16 items, eight to assess cognitive symptoms, and eight for somatic symptoms related to an increased arousability tendency at night [20]. Each item is rated using a 5-point Likert scale from 1 (‘not at all’) to 5 (‘frequently’). The PSAS has been widely used in patients with insomnia, and controls. Positive screening for cognitive symptoms was considered in those cases with a score ≥20, and for somatic symptoms when the score was ≥14.
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) is a validated, and widely used questionnaire, designed in 1988 by Buysse and collaborators, which allows to evaluate sleep quality, and disturbances in the last month [21]. The questionnaire includes twenty-four queries. Nineteen of these items are self-rated, and generate seven sleep components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping medication, and daytime disturbance. Scores for each question are weighted equally from 0–3 score, with higher scores indicating more acute sleep disturbances. A global score >5 provides a high sensitivity and specificity (89.6% and 86.5%, respectively) to identify poor sleepers.
Healthy habits
Finally, the third section included few questions regarding healthy habits during the pandemic such as sunlight exposure, and physical activity. Regular sunlight exposure was considered in those cases whose light exposure was 15–30 minutes, ≥4 days/week, and regular physical activity when they practiced exercise for 20–30 minutes, at least 2–3 days/week.
Statistical analysis
Statistical analyses were performed using SPSS, version 15 (SPSS Inc., Chicago, IL, USA). Results were summarized by means, and standard deviations for continuous variables such as age, stress, hyperarousability scores, PSQI components, and global scores, and percentages for continuous or categorical variables such sex, personal living situation, professional information, frequency of moderate-severe stress (score ≥14), frequency of anxiety, and depression, frequency of positive screening for somatic, and cognitive symptoms, frequency of poor sleepers, and frequency of healthy or unhealthy habits. The t-student was conducted to examine differences between the main continuous variables, and chi-square to investigate differences between categorical variables. The study population was divided into three groups according to time of assessment and attended patients (group 1: baseline, healthcare workers in charge of non-COVID patients, group 2: baseline, healthcare workers in charge of COVID-19 patients, and group 3: follow-up, healthcare workers who attended COVID-19 patients). Group 1 and 2 were compared to investigate the short-term impact of COVID-19 exposure, while comparing group 2 and 3 we assessed the medium-term impact of the pandemic on mental health and sleep. Differences were considered statistically significant when p<0.05.
RESULTS
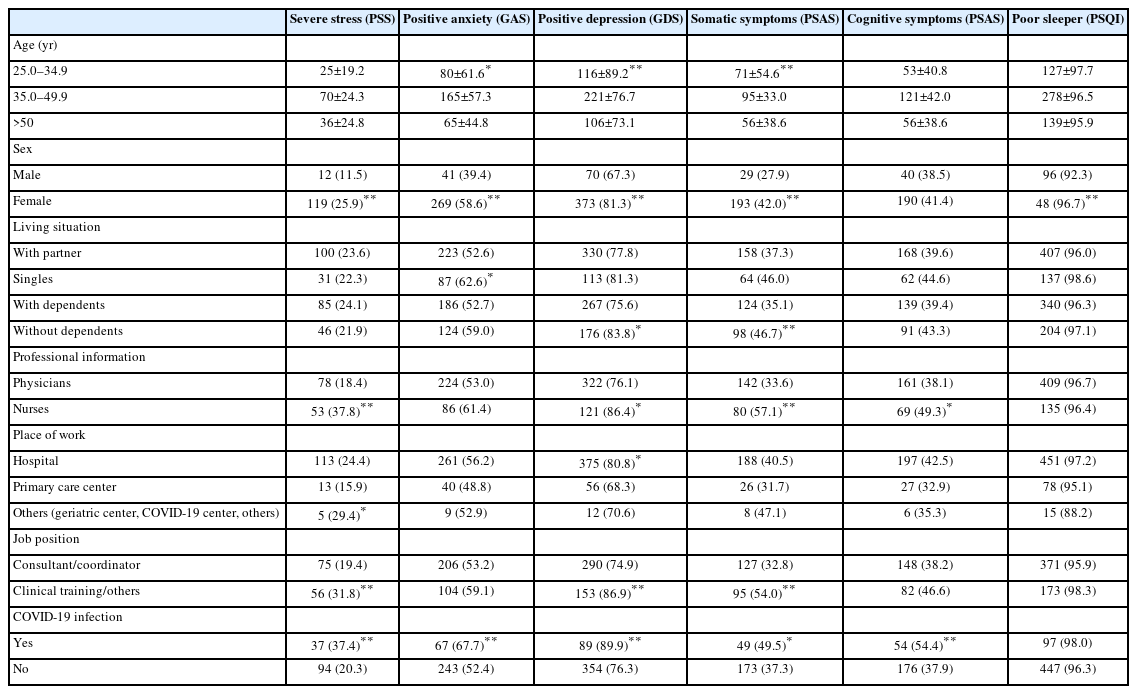
Overall, 563 questionnaires were included. Of them, 425 were completed during the baseline period, and 138 corresponded to the follow-up assessment, at least 6 months later after the first evaluation (Figure 1). All data generated or analyzed during this study are included in this published article. The main characteristics of the study sample are shown in Table 1. Eighteen per cent of Spanish HCP had COVID-19 infection.
Stress, mental health, and poor sleep
In the study population, most healthcare providers reported moderate-severe stress (98.1%). Positive screening for anxiety, and depression was identified in 55.1% and 78.7% of participants respectively, and poor sleep quality in 96.6%, according to the global score of PSQI. Finally, the frequency of somatic, and cognitive-PSAS symptoms were 39.4% and 40.9% respectively.
Statistically significant differences of the frequency of stress, mental health, and sleep problems were found according to social, demographic, and occupational characteristics of the study population. For instance, the younger group of HCP (25.0–34.9 years) had a higher frequency of anxiety (p=0.012), depression (p=0.003), and somatic symptoms of hyperarousability (p<0.001) compared to the two older groups. In the same way, women compared to men reported more frequently severe stress (p=0.003), anxiety (p<0.001), depression (p=0.002), somatic symptoms (p=0.008), and poor sleep quality (p=0.007). Regarding the personal living situation, the frequency of positive screening for anxiety was higher in singles compared to those who had partner (p=0.040). Interestingly, HCP with dependents (children or parents) had a lower frequency of depression (p=0.022), and lower somatic symptoms (p=0.007) compared with those without dependents at home. Nurses compared to physicians reported more frequently severe stress (p<0.001), depression (p=0.010), somatic (p<0.001), and cognitive symptoms (p=0.019). Similarly, Spanish HCP who worked in hospitals during the pandemic had a higher frequency of depression symptomatology (p=0.027). While less experience or responsibility at work was associated to an elevated prevalence of severe stress (p=0.005), depression (p=0.001), and somatic symptoms (p<0.001). HCP who reported history of COVID-19 infection had more frequently severe stress (p=0.001), anxiety (p=0.005), depression (p=0.003), somatic (p=0.024), and cognitive-PSAS symptoms (p=0.002). As it was expected, poor sleep quality was reported more frequently by patients with anxiety (56.3%. vs. 43.8%, p=0.002) and depression (79.6% vs. 20.4%, p=0.005) compared with those without mental health symptomatology (Table 2). Finally, no statistically significant differences in the frequency of anxiety were found between the different work (p=0.093) or rest schedules (p=0.257), neither for depression (p=0.592, and p=0.086).
Differences of the main variables between the case and the control groups
First, we investigated general differences between HCP in charge of non-COVID and COVID patients, group 1 and 2 respectively, at baseline assessment. The prevalence of COVID infection was almost three-fold higher in group 2 compared to group 1 (p=0.001). HCP in charge of COVID patients were younger compared to professionals in charge of patients with other pathologies (p=0.002). Second, we assessed the short-term impact of COVID-19 exposure at work in mental health and sleep quality. Differences were statistically significant between the case and the control group at the baseline assessment for the mean score of the PSS (p=0.005), the frequency of anxiety (p=0.002), the frequency of depression (p=0.001), the frequency of somatic-PSAS symptoms (p=0.037), and the global score of the PSQI (p=0.019), but not for cognitive-PSAS symptoms, neither for poor sleep frequency (Table 3 and Figure 2). Interestingly, group 2 reported a longer work schedule (of 12 hours or more in 41.4% of subjects) compared to group 1 (16.5%, p<0.001), and shorter rest schedule compared to the control group (2 or more days: group 2: 83.6% vs. group 1: 93.1%, p=0.002).
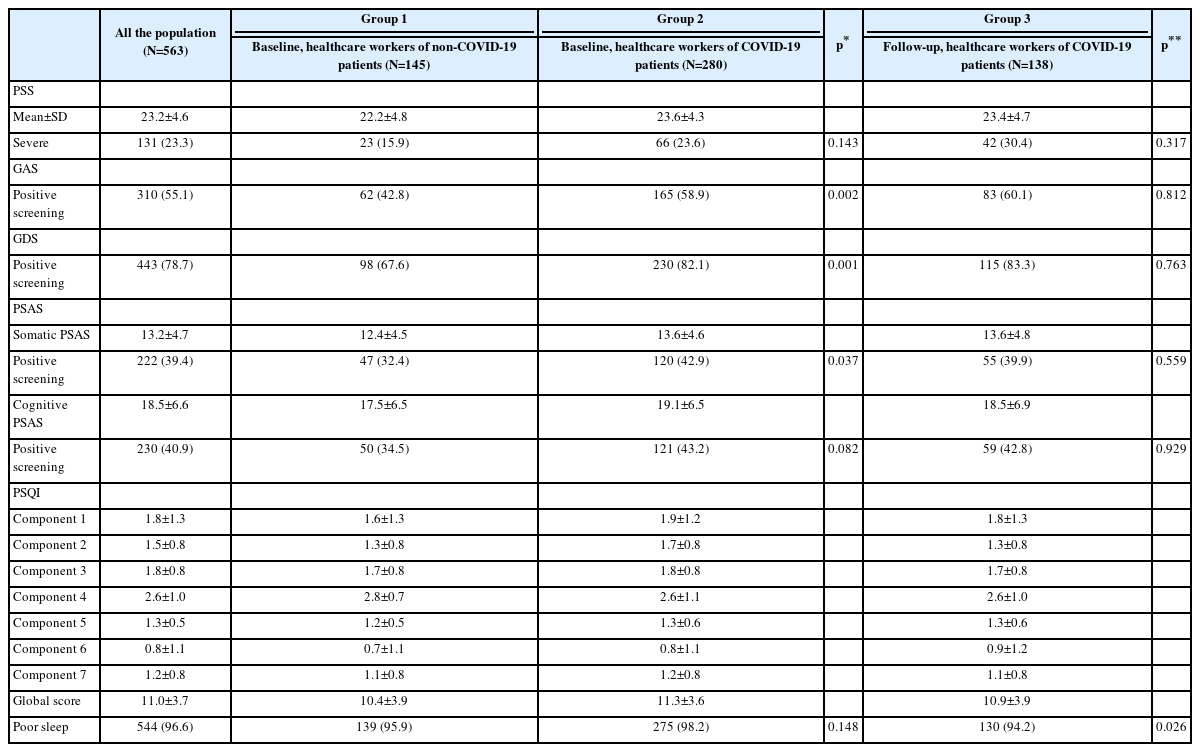
Summary of stress, mental health, somatic and cognitive symptoms, and sleep quality in the different groups of study sample
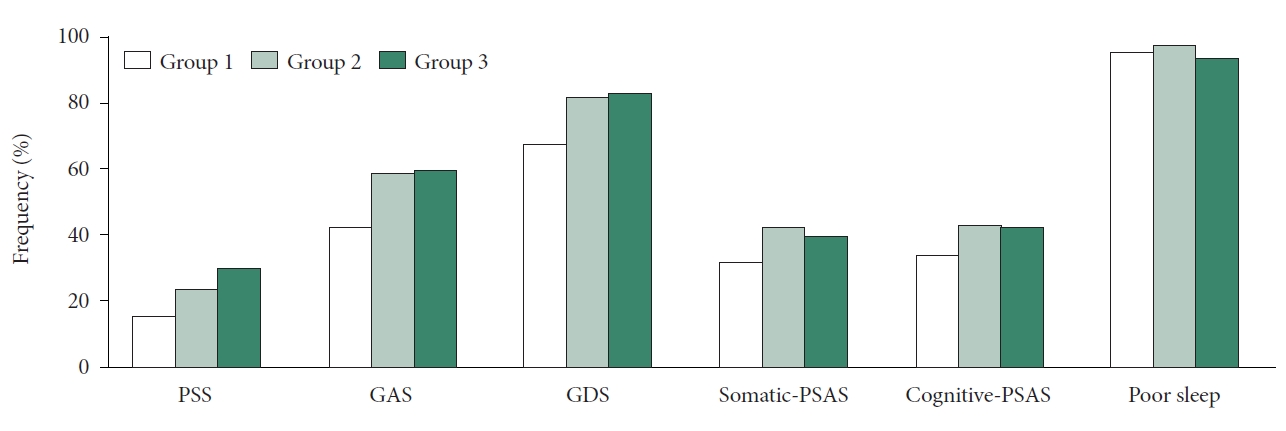
Summary of the frequency of main variables in the different groups of the study sample. Group 1 (white): baseline, healthcare workers of non COVID-19 patients, group 2 (light green): baseline, healthcare workers of COVID-19 patients, group 3 (dark green): followup, healthcare workers of COVID-19 patients. Poor sleep according to the PSQI. PSS, Perceived Stress Scale; GAS, Goldberg Anxiety Scale; GDS, Goldberg Depression Scale; PSAS, Pre-Sleep Arousal Scale; COVID-19, coronavirus disease-2019; PSQI, Pittsburgh Sleep Quality Index.
Finally, we compared group 2 and 3 to investigate the persistence of the negative impact of COVID-19 exposure at work overtime. No differences were found in the mean score of PSS or frequency of severe stress, neither for anxiety, depression, somatic or cognitive symptoms. Nevertheless, the frequency of poor sleep (p=0.026) was higher in group 2 compared to group 3. Between the two case groups (2 and 3) longer work schedule was reported at the beginning of the pandemic than in the follow-up (≥12 hours/day; group 2: 41.4% vs. group 3: 26.1%, p=0.001), and shorter rest time at the baseline assessment as well (2 or more days; group 2: 83.6% vs. group 3: 94.2%, p<0.001).
Differences in the frequency of mental health disorders according to healthy habits
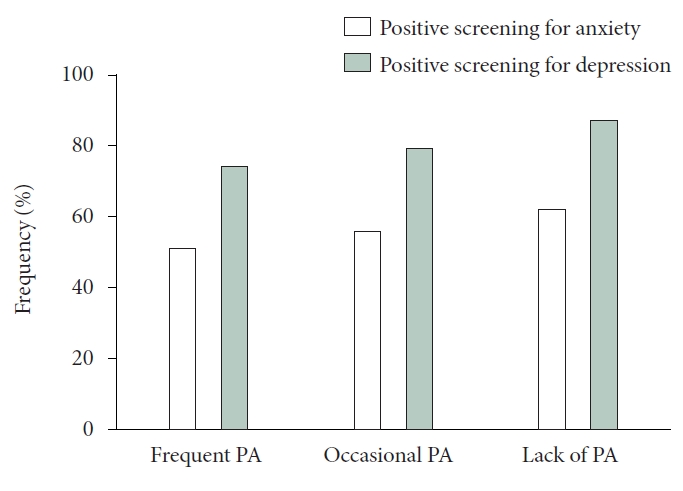
No statistically significant differences were found in the frequency of sunlight exposure or physical activity between the three groups of the study population. However, a decrease in the frequency and regularity of sunlight exposure was associated to an increase of positive screening for anxiety (p=0.001), and for depression (p=0.002) (Figure 3). While a decrease in the frequency and regularity of physical activity was associated to an increase of positive screening for depression (p=0.019), but not for anxiety (Figure 4).
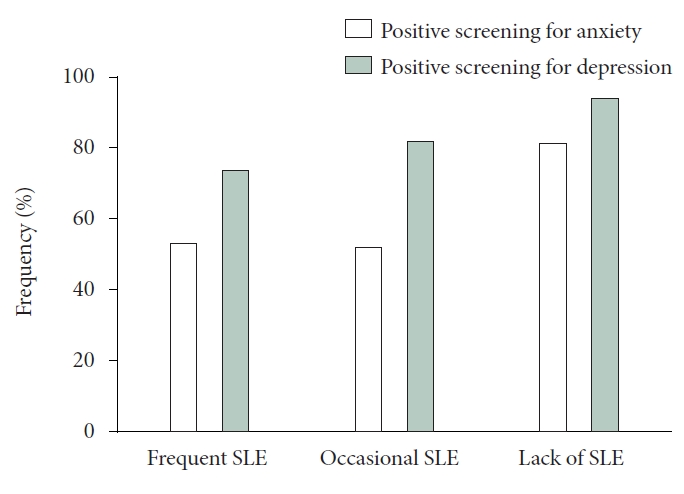
Frequency of anxiety and depression according to SLE. Frequent SLE: 15–30 minutes ≥4 days/week, occasional SLE: <15 minutes <4 days/week, lack of SLE: practically not SLE. SLE sunlight exposure.
DISCUSSION
Results of this case-control, and follow-up study show that most Spanish HCP were exposed to a persistent stress overtime, and not only at the beginning of the pandemic. In addition, the frequency of perceived stress was higher in the group of HCP in charge COVID-19 compared to the control group in baseline assessment. Sociodemographic and professional factors such sex, nursing professionals, and less experience or responsibility at work were also associated to an increase of work-stress related, as it had been reported in previous studies, performed during the first peak of the COVID-19 pandemic, and even before of this period [22-25].
During the outbreak of the severe acute respiratory syndrome (SARS) in 2003 about 35% of HCP had psychological comorbidities [26]. Results of the present study shows that 55% of Spanish HCP reported anxiety, 79% symptoms of depression, 97% poor sleep, and about 40% somatic, and cognitive-PSAS symptoms. These data are high compared to previous studies performed at the beginning of the COVID-19 pandemic [15,27]. The study of Dosil Santamaría et al. [15] reported that 47% of Spanish HCP suffered stress, 37% anxiety, 27% depression and 29% sleep problems. Similar results were found by Muller et al. [27] This Norwegian review estimated that the mean for anxiety was 21%, 24% for depression, and 37% for sleep problems. The elevated rates for mental health problems in the present study can obey to different reasons. First, the high frequency of females, nurses, and young healthcare personnel in charge of COVID-19 patients, three groups with high risk for mental health problems. Moreover, it is possible that these groups with elevated symptomatology may be more willing to participate. Other factors to take into account are tools used to assess psychological impairment, that can differ from previous studies. Finally, results of this study are also difficult to compared to other research investigations focused on the first peak of the pandemic. In fact, to our knowledge, only one longitudinal study has investigated mental health in HCP in Spain [17]. This study, that examined differences of symptoms during the first peak of the COVID-19 pandemic and immediately after, also found an early increase on mental health problems by the end of first peak of the pandemic. In addition, it is probably that mental health problems before of the pandemic in Spanish HCP were underestimated. In fact, Irigoyen-Otiñano et al. [28] in a study performed from 2005 to 2013 showed that Spanish physicians had a higher suicide rate compared to general populations.
On the other hand, we were also interested to assess whether good habits such as physical activity or sunlight exposure can impact on mental health in Spanish HCP during the COVID-19 pandemic. Interestingly, results of the present study found that sunlight exposure decreased anxiety, and depression symptoms. While regular physical activity decreased depression symptoms. Therefore, it appears that healthy habits could have a positive impact on mental health of HCP even in this overwhelming period of maximum stress such it was suggested by Tovani-Palone et al. [29] in an article about the importance of healthy habits during the COVID-19 pandemic for general populations. These results are interesting, because a Spanish cross-sectional study about life habits of HCP during the third wave of COVID-19 found changes in sleep quality, eating behavior, and unhealthy habits such an increase of alcohol, tobacco, and drug consumption [30].
Several strengths should be noted. First, the recruitment process, based on on-line questionnaires allowed us to study health personnel from different places of Spain from the beginning of the pandemic. Second, this is a case-control and longitudinal study. To our knowledge, up to now, only one longitudinal study has been published about mental health in Spanish HCP during the pandemic. However, the follow-up period in the previous research was short compared to the present study [17]. Third, assessment of stress, psychological disorders, poor sleep, and hyperarousability were based on five validated scales. Fourth, results of the present study will allow us to understand better the mental health of our health system by the end of pandemic. Finally, the impact of healthy habits on psychiatric disorders were also investigated in the present study. Despite these strengths, the study has several limitations. First, the recruitment process was based on self-applied online survey. Although, this could be considered a limitation, this recruitment process allows us to collect psychological symptoms in health personnel in periods of high work-related pressure, increase the sample size, and improve cost-effectiveness. Results of the present study should not be generalized due to the heterogeneity of the research sample throughout the Spanish geography, and the elevated frequency of females in the present study, a risk factor for mental health, and sleep problems.
In summary, stress, mental health, and sleep problems were common in Spanish HCP, especially in those in charge COVID patients. These findings persisted throughout the pandemic. Healthy habits appear to have positive impact in mental health. Further studies to investigated mental health, and insomnia in the post-pandemic period in HCP are needed.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Seockhoon Chung, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Marta Moraleda-Cibrián. Data curation: Marta Moraleda-Cibrián. Formal analysis: Marta Moraleda-Cibrián. Funding acquisition: Marta Moraleda-Cibrián. Investigation: Marta Moraleda-Cibrián. Methodology: Marta Moraleda-Cibrián. Project administration: Marta Moraleda-Cibrián. Resources: Marta Moraleda-Cibrián. Supervision: Seockhoon Chung. Writing—original draft: Marta Moraleda-Cibrián. Writing—review & editing: all authors.
Funding Statement
This study was supported by the Spanish Sleep Society (SES Research Award 2020).
Acknowledgements
We thank all the Spanish healthcare professionals who participated in the present study.