The Korean Version of the Body Image Scale-Reliability and Validity in a Sample of Breast Cancer Patients
Article information
Abstract
Objective
The Body Image Scale (BIS) developed in collaboration with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Study Group is a brief questionnaire for measuring body image concerns in patients with cancer. This study sought to assess the reliability and validity of the Korean version of the Body Image Scale (K-BIS).
Methods
The participants consisted of 155 postoperative breast cancer patients (56 breast conserving surgery, 56 mastectomy, and 43 oncoplastic surgery). Subjects were evaluated using the K-BIS, the Body-Esteem Scale for Adolescents and Adults (BESAA), the Rosenberg Self-Esteem Scale (RSES), the Hospital Anxiety and Depression Scale (HADS), and the World Health Organization Quality of Life Scale Abbreviated Version (WHOQOL-BREF). Test-retest reliability and internal consistency were examined as a measure of reliability and validity was evaluated by convergent validity, discriminant validity and factor analysis.
Results
Cronbach's α value was 0.943. The total score of the K-BIS was negatively correlated with the BESAA (r=0.301, p<0.001) and the body image facet in the WHOQOL-BREF (r=0.315, p<0.001). The total score of K-BIS positively correlated with the HADS (HAD-A: r=0.501, p<0.001, HAD-D: r=0.466, p<0.001). As for determining discriminant validity, scores were compared between the BCS subgroup, mastectomy subgroup, and oncoplastic surgery subgroup. Difference between the mastectomy subgroup and oncoplastic surgery subgroup was statistically significant (p=0.017). Factor analysis resulted in a single factor solution in three out of four anlyses, accounting for >59% variance.
Conclusion
The K-BIS showed good reliability and validity for assessment of body image in Korean breast cancer patients.
INTRODUCTION
Breast cancer has become the most common cancer in women throughout the world.1 Similarly, the number of patients with newly diagnosed breast cancer increased 2.5-fold in recent 8 years and breast cancer became the second most common cancer in women in Korea.2 The number of women who survive breast cancer has increased significantly in recent years, with the progresses in diagnosis and treatment. In 2005, five-year survival rate of women with breast cancer has climbed to 90% compared to 1995 in United States.3 As survival times increase, an important goal for breast cancer patients and survivors is to improve their quality of life and reduce the adverse effect.4
Women who are treated for breast cancer are exposed to marked alterations in their physical appearance, such as loss or disfigurement of breast, scars from surgery, skin changes related to radiotherapy, and hair loss due to chemotherapy. And these marked alterations lead to marked alteration in their body image.5,6 Body image is an important component of a cancer patient's quality of life, having a relevant role on their adjustment to the disease.5,7-9 Women with better body image perceptions had higher levels of self-confidence in coping with breast cancer.10 On the other hand, Poorer body image is associated with poorer self-rated health, chronic fatigue and mental distress, and poorer generic and disease-related quality of life.6 Therefore body image is an important component of the quality of life assessment, but a review of the literature revealed the lack of a suitable scale to measure body image in cancer patients, particularly in the clinical trials setting.5,11
Considering this, it is clear that a brief and psychometric robust instrument, applicable to all cancer patients, independent of age, cancer type, treatment or stage of the disease, is needed to assess body image, both in clinical and research settings. The body image scale (BIS), developed by Hopwood et al. fulfils these criteria, allowing a complete yet brief assessment of behavioral, affective and cognitive aspects of body image and is also sensitive to typical areas of concern for cancer patients. The development of this instrument followed similar guidelines to those recommended by the Quality of Life Study Group from the European Organisation for Research and Treatment of Cancer (EORTC) for questionnaire module development12 and was designed to be used along with the core Quality of Life Questionnaire (QLQ-C30) or other Quality of Life (QOL) measure, complementing QOL assessment in clinical trials or psychosocial research. The scale was validated among breast cancer patients and has revealed good psychometric properties, proving to be an adequate and valid measure of body image among this population.5 According to the authors, it is also applicable across several types of cancer and treatment situations.
In Korea, a validated measure of body image specifically designed for cancer patients has not yet been developed thus limiting research in this area. In this study, we aimed to develop and validate a Korean version of the Body Image Scale (K-BIS) in a sample of breast cancer patients, to evaluate its potential for application in Korean subjects. Therefore, this study was conducted to analyze the reliability and validity of the Korean version of the Body Image Scale (K-BIS) among a sample of breast cancer patients.
METHODS
Participants
The subjects consist of 155 postoperative breast cancer patients, participating in a larger study of psychosocial adjustment carried out by 'Mental health assessment and support Team (MHAST) for breast cancer' of the Kyungpook National University Hospital (KNUH) and Kyungpook National University Medical Center (KNUMC) in the comprehensive medical team of Breast cancer center. A group of newly diagnosed breast cancer patients who were admitted to the KNUH and KNUMC were enrolled following their surgery between July 2010 and December 2011. Interested patients were eligible to participate if they met the following inclusion criteria: having been diagnosed breast cancer, having done breast surgery, having no other major disabling medical or psychiatric conditions, being female aged between 18 and 80 years, and able to give written informed consent, and able to read and write Korean. The sample consisted of 155 patients: the three patient samples contributing to the analysis were 56 women treated by breast conserving surgery (BCS), 56 women treated by mastectomy, and 43 women treated by oncoplastic surgery (breast cancer surgery with immediate breast reconstruction). Women diagnosed with invasive ductal carcinoma comprised the majority of the sample (78.1%) and the mean age of participants was 49.9 years [standard deviation (SD)=8.79] (Table 1). This study was approved by the institutional review board of Kyungpook National University Hospital. All participants provided written informed consent after the study had been fully explained.
Assessment
Body Image Scale
The Body Image Scale (BIS) is a self-reporting scale and a 10 item measure developed to quickly and comprehensively assess affective (e.g., feeling self-conscious), behavioral (e.g., difficulty looking at the naked body) and cognitive (e.g., satisfaction with appearance) dimensions of body image in cancer patients and has been designed to use with any cancer or the treatment thereof. It uses a 4-point response scale (0=not at all to 3=very much) and the final score is the sum of the 10 items, ranging from 0 to 30, with zero representing no symptoms or distress and higher scores corresponding to increasing distress and concnerns of body image. The BIS revealed a single-factor solution and demonstrated good psychometric characteristics with adequate reliability (Cronbach's α=0.93) and adequate validity.5
Body-Esteem Scale for Adolescents and Adults
The Body-Esteem Scale for Adolescents and Adults (BESAA) assesses participants' attitudes and feelings about their bodies and appearances. This scale is a 23-item self-report measure. The 23-item BESAA is an easy-to-administer, psychometrically sound instrument that taps three aspects of Body-Esteem in adolescents and adults: 1) general feelings about appearance, 2) weight satisfaction, and 3) attributions of positive evaluations about one's body and appearance to others. Respondents indicate their degree of agreement on a 5-point Likert scale ranging from 0 (never) to 4 (always), and negative items are reverse scored.13 Item ratings are summed to yield a total score ranging from 0 to 92; higher scores indicate higher body esteem. We used the Korean Version of the BESAA. The Korean version of the BESAA has been shown to have a good reliability (Cronbach's α=0.90, test-retest reliability coefficient r=0.66).14
Rosenberg Self-Esteem Scale
The Rosenberg Self-Esteem Scale (RSES) assesses global attitudes toward the self (i.e., the sense of self-worth and self acceptance).15 This scale is a 10-item self-report measure. Items are rated on a 4-point Likert scale (1=strongly disagree, 4=strongly agree). Item ratings are summed to yield a total score that ranges from 10 to 40; higher scores indicate higher self esteem. The RSES demonstrates high reliability with adolescent boys and young adult samples. Cronbach's α values were 0.88 for the English version and 0.79 for the Korean version.16
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) is a 14-tiem self-report screening scale that was originally developed to indicate the possible presence of anxiety and depression states in the setting of a medical nonpsychiatric outpatient clinic.17 HADS consists of a 7-item anxiety subscale (HAD-A) and a 7-item depression subscale (HAD-D). Each item scores on a 4-point Likert scale, giving maximum subscale scores of 21 for depression and anxiety, respectively. The norms give us an idea of the level of Anxiety and Depression (0-7=normal, 8-10=borderline abnormal, 11-21=abnormal). The Korean version of HADS was used in this study and it has been shown to have a good internal consistency. Cronbach's α values were 0.89 for the HAD-A and 0.86 for the HAD-D.18
World Health Organization Quality of Life Scale Abbreviated Version
To measure the individual's subjective perception of QOL, we used the Korean version of the World Health Organization Quality of Life Scale Abbreviated Version (WHOQOL-BREF). This instrument was validated for the Korean population according to guidelines of the WHOQOL group and presented good reliability and validity. It is comprised of 26 items providing scores for four domains, each one comprising several specific facets: physical, psychological, social relationships, and environment, including a facet of the overall QOL (general QOL and general health). It employs a 5-point scale in which higher scores indicate higher QOL. The Korean version of WHOQOL-BREF has been shown to have a good internal consistency. (Cronbach's α=0.898). Cronbach's α values ranged, in the Korean version, from 0.583 (domain 3) to 0.777 (domain 1) between domains.19
Procedures
The Korean version of the Body Image Scale (K-BIS) was developed through a forward-backward translation procedure, according to the EORTC Quality of Life Group Translation Procedure. In advance, we got the permission from the author of the BIS about the translation. The authors of the Korean version, who are native speakers of Korean with a high level of fluency in English, independently translated the 10 items of the English version of the BIS. Both translated versions were then compared and after discussing and analyzing its similarities and differences, the first Korean version was obtained. A native English speaker subsequently translated the preliminary Korean version back to English without reference to the BIS. Finally, the two versions (the BIS and the back translated) were compared and translation difficulties were analyzed and resolved between the translators in order to attain a comprehensible instrument that is conceptually consistent with the BIS. When translating and adapting this instrument, the specific Korean culture and language was taken into account. Maintaining the consistency with the BIS at all times, some expressions or phrases were slightly altered in order to make them as clear as possible for Korean patients.
The preliminary Korean version was administered to a pilot group of 15 breast cancer patients in order to identify and solve any potential problems in translation. After completing the questionnaire, patients were asked about the each item. In general, patients showed a good understanding of items and had no major difficulties in responding to the questionnaire. The final Korean version of the Body Image Scale (K-BIS) was then attained (Supplement 1).
Statistical analysis
Descriptives were obtained for all demographic and clinical characteristics, both for the global sample as for the surgical subgroups. One-way analysis of variance (ANOVA) and Scheffe test for post hoc test were used to explore differences between the subgroups. According to the recommendations of Hopwood et al.5 missing scores in one or two items of the K-BIS were replaced by the mean of the items to which participants had responded. To assess reliability and internal consistency, item-total item correlation was assessed using Cronbach's α coefficient, as well as corrected item-total correlations and alpha values when the item was deleted. Test-retest reliability was calculated using Pearson's correlation coefficient. To explore the construct validity, Pearson's correlations between the K-BIS and other measures (the BESAA, the RSES, the HADS, the WHOQOL-BREF) were calculated. To further analyze the discriminant validity of the K-BIS, differences between the types of surgeries were analyzed through one-way ANOVA and Scheffe test for post hoc test. And we also conducted the analysis of covariance (ANCOVA) to control the variables may affect the K-BIS scores of patients in each subgroups. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS) software platform for Windows, version 18.0. All statistical tests were two-tailed.
RESULTS
Demographic and clinical characteristics
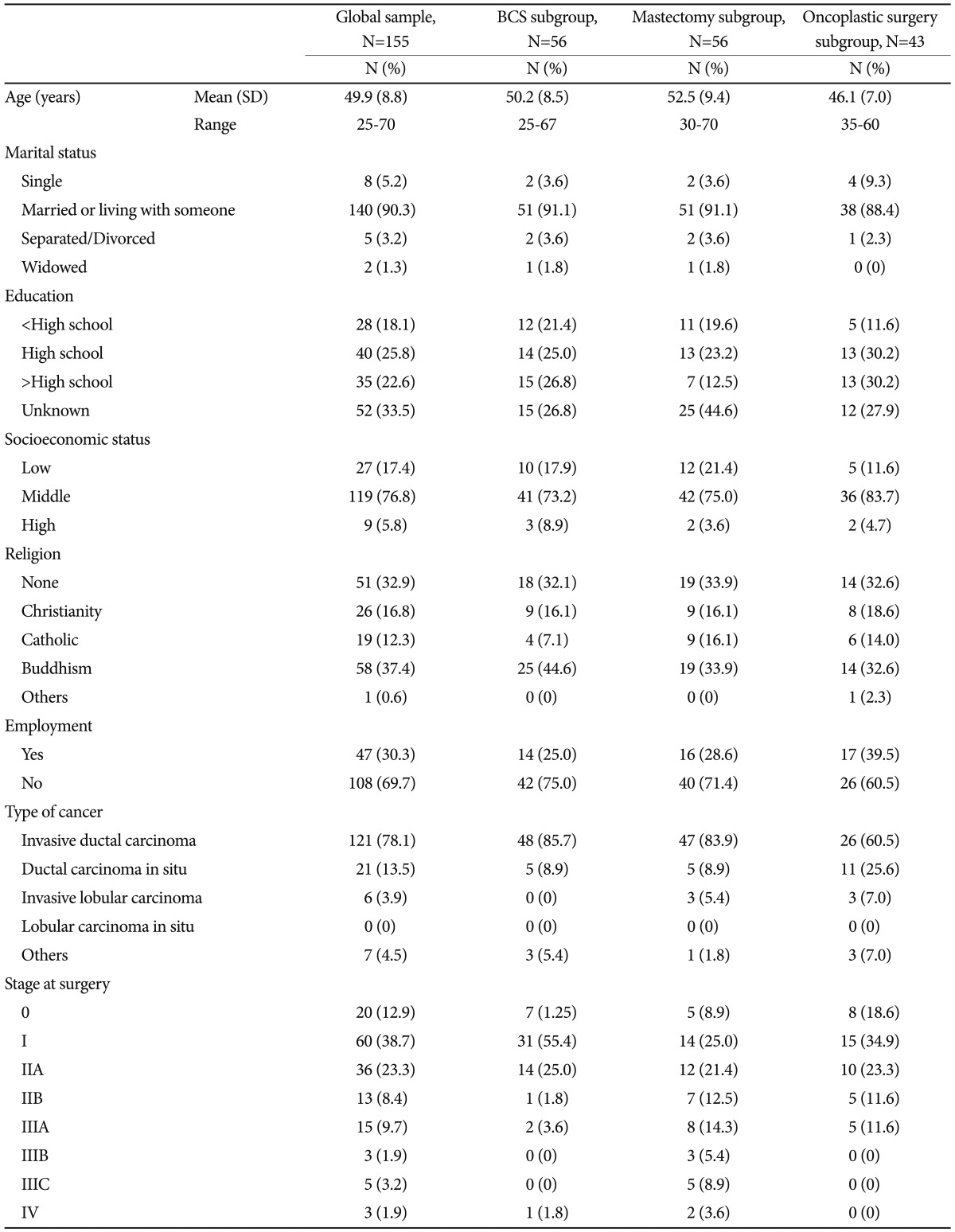
The sample consisted of 155 patients: the three patient samples contributing to the analysis were 56 women treated by breast conserving surgery (BCS), 56 women treated by mastectomy, and 43 women treated by oncoplastic surgery (breast cancer surgery with immediate breast reconstruction). The surgical subgroups were similar in terms of the main demographic and clinical characteristics. Nevertheless, the ANOVA revealed that patients treated with mastectomy presented a higher mean age (mean age=52.5, SD=9.4, range=30-70) than those who had treated with oncoplastic surgery (mean age=46.1, SD=7.0, range=35-60). It was statistically significant in the post hoc test (p=0.001). And the ANOVA revealed that patient treated with mastectomy presented the more advanced mean stage at surgery than those who had treated with BCS or oncoplactic surgery. It was also statistically significant in the post hoc test. The p values are 0.000 and 0.003, respectively. Other demographic and clinical characteristics are shown in Table 1.
Reliability
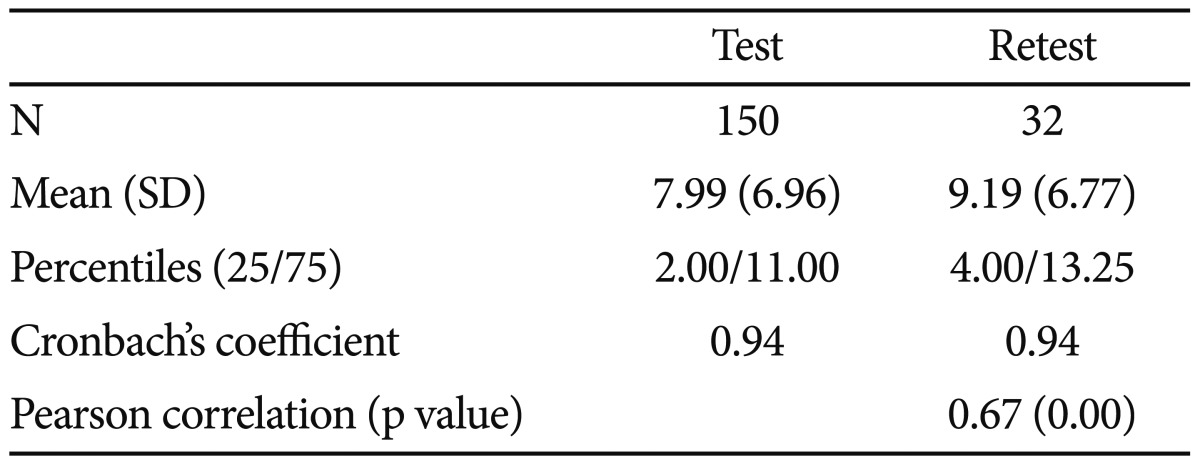
Cronbach's α value revealed that the K-BIS has adequate internal consistency, in the total sample (Cronbach's α=0.943), as in the subgroups of BCS (Cronbach's α=0.925), mastectomy (Cronbach's α=0.961) and oncoplastic surgery (Cronbach's α=0.919). In the global sample, corrected item-total correlations ranged from 0.52 to 0.91. All the items did not increase the alpha value when the items were deleted. For the 32 participants who completed the K-BIS on two occasions with a 6-months interval, the test-retest reliability, as measured by Pearson's r correlation coefficient, was r=0.67 (p<0.001)(Table 2).
Convergent validity
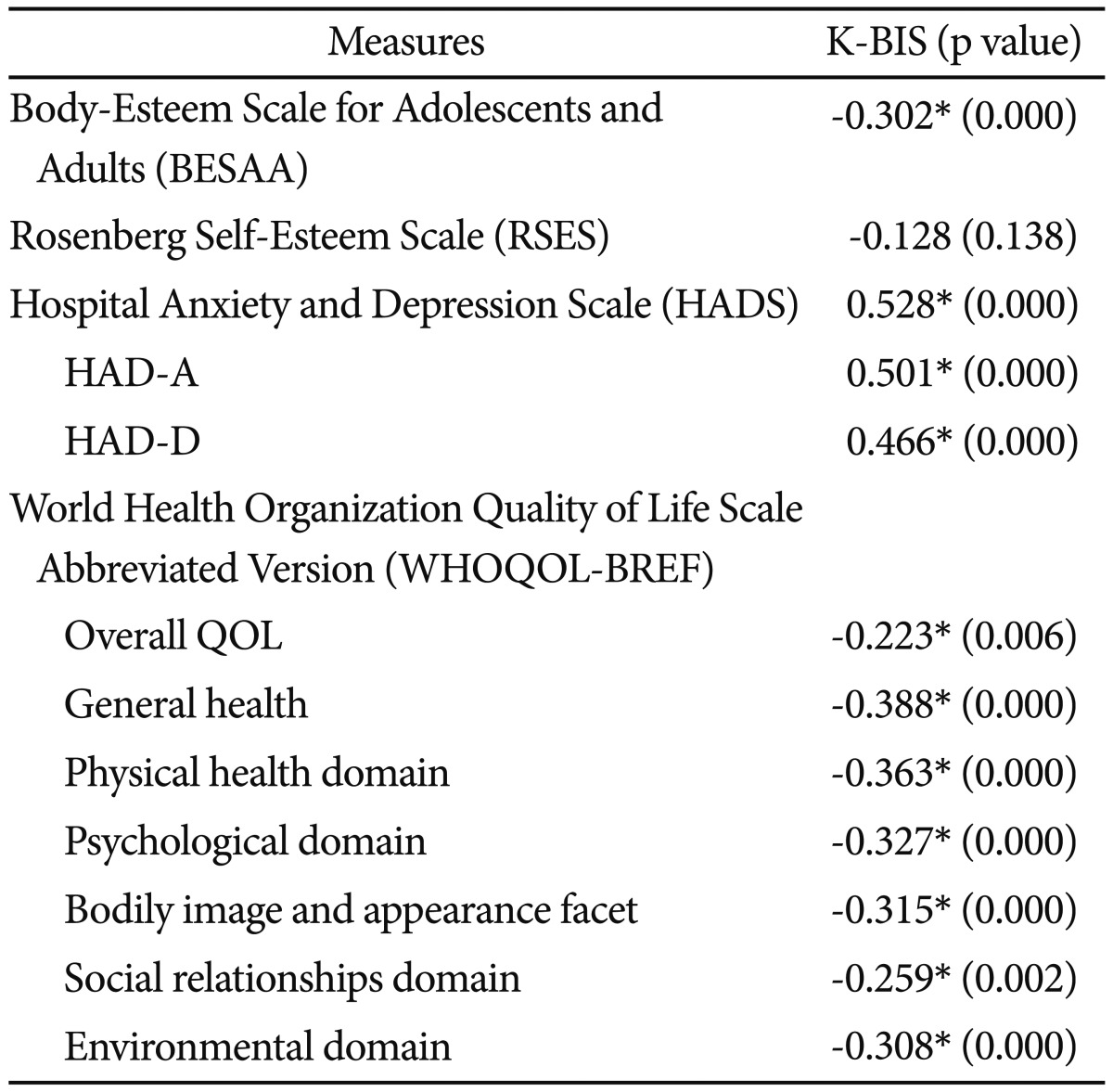
Convergent validity was assessed by comparing the K-BIS with the BESAA, the RSES, the HADS, and the WHOQOL-BREF. All the WHOQOL domains were analyzed as well as the specific facets of body image. The total score of the K-BIS was negatively correlated with the BESAA (r=0.301, p<0.001) and all of the domains of the WHOQOL-BREF, as well as the specific facet of body image facet (r=0.315, p<0.001), included in the psychological domain. The total score of K-BIS positively correlated with the HADS (HAD-A: r=0.501, p<0.001, HAD-D: r=0.466, p<0.001). However, there was no statistically significant correlation between K-BIS and the RSES (Table 3).
Disciminant validity
The discriminant validity of the K-BIS was further assessed by comparing the K-BIS scores of patients who were treated by BCS (n=55), those treated by mastectomy (n=53), and those treated by oncoplastic surgery (n=42). We excluded 5 subjects due to missing data in at least 3 item on the K-BIS. In each group, the numbers of excluded subjects are 1, 3, and 1, respectively. The ANOVA [F(2,147)=4.622, p=0.011] revealed that patients who were treated by mastectomy (M=10.17, SD=8.22) presented significantly more body image concerns than those treated by BCS (M=7.33, SD=6.26) or Oncoplastic surgery (M=6.10, SD=5.31). However, the statistical significance existed only between the mastectomy and oncoplastic surgery subgroups (p=0.017). And we conducted the ANCOVA to adjust the differences of age and stage at surgery among the subgroups. The ANCOVA revealed that the differences of age and stage at surgery didn't affect the K-BIS scores of patients (p=0.690, p=0.084). And there were statistically significant score differences of K-BIS among the subgroups (p=0.007, p=0.035).
Factor analysis
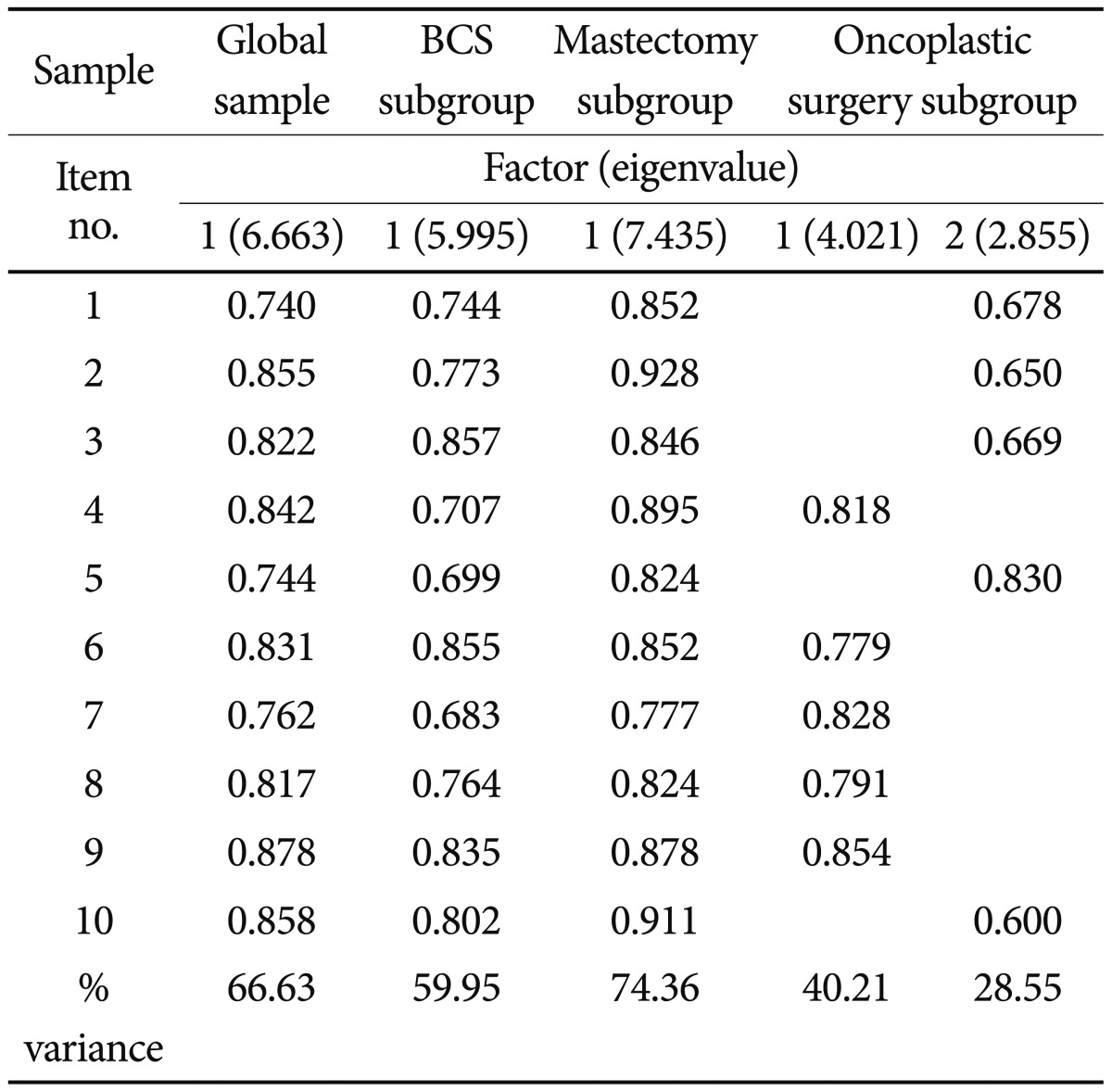
Scale structure was examined using General Least Squares Factor Analysis on the Global sample and on the component subgroups, namely the BCS, mastectomy and oncoplastic surgery subgroup. These analyses showed a generally consistent structure between samples with a single factor solution in the global sample, BCS subgroup, and mastectomy surgery subgroup analyses explaining 66.63, 59.95 and 74.36% of the variance, respectively as shown in Table 4. Factor analysis on the oncoplastic surgery subgroup resulted in a two-factor solution, in which the scale items 4, 6-9 explained 40.21% of the variance and items 1-3, 5, 10 explained 28.55% of the variance. Table 4 shows the factors with their eigenvalues and the percentages of variance explained by each.
DISCUSSION
In the present study, we found that the K-BIS exhibited good reliability and validity. Internal consistency of the K-BIS was adequate in the global sample (Cronbach's α=0.943); this coefficient was within the optimal range for this value and consistent with the Cronbach's α of 0.93 in the global sample, reported for the original BIS. Cronbach's α statistics for the K-BIS in the surgical subgroups were quite similar to those reported for the original BIS (i.e., 0.91 for patients treated with breast conserving surgery, 0.91 for patients treated with mastectomy). The internal consistency of the scale was also confirmed by the item-total correlations, all above the usual criteria of 0.30,20 which indicates that all items correlate well with the total scale score and measure the same construct. Moreover, all the Cronbach's α values for each deleted items were lower than the overall Cronbach's α, indicating that the deletion did not contribute to an increase of the overall reliability.
Scale structure was examined using General Least Squares Factor Analysis on the global sample and on the component subgroups which consisted of women treated by BCS, mastectomy and oncoplastic surgery. These analyses showed a generally consistent structure between samples with a single factor solution in the global sample, BCS subgroup, and mastectomy surgery subgroup analyses explaining 66.63, 59.95 and 74.36% of the variance, respectively. However, the factor analysis on the oncoplastic surgery subgroup result gave a two factor solution. When the authors of the original BIS found a two factor solution in the subsample of patients treated with mastectomy, they considered that the two factor solution in the smaller mastectomy dataset gave an understandable result, but one that was not reproducible.5 Therefore, our factor analysis confirmed that the scale is a unitary measure in all but one analysis. It replicated and extended previous findings to the original scale.
K-BIS scores were negatively correlated with other measures of body image. Particularly, the K-BIS was correlated with the Body-Esteem Scale for Adolescents and Adults (BESAA) and the body image facet of the psychological QOL domain moderately, which suggests that this measure covers the issues such as body shame, self-consciousness of appearance and global satisfaction with physical appearance, as originally intended. This finding is consistent with other studies that have demonstrated that women who tend to base their self-worth and self-esteem on their appearance also tend to be more concerned with their body image.21,22
However, in the present study, K-BIS scores were not correlated with the Rosenberg Self-Esteem Scale (RSES) that assesses global attitudes toward the self. This finding is also not consistent with the other validation study of BIS in Portugal.23 In this study, all the assessments were taken within two weeks after surgery unlike the Portuguese study. The two weeks is too short period to affect global attitudes toward the self of patient. It is possible that this result is caused by the time point all the assessments were taken. The follow up study is in progress. We anticipate that the correlation between K-BIS and RSES will be exposed much clearer in the follow up study.
Concerning the pattern of associations between the K-BIS scores and the WHOQOL-BREF domains and general facet, our findings showed medium to large correlations between them. This calls our attention to the importance of body image on a patient's QOL and consistence with previous findings showing that more concerns with appearance are related to lower levels of QOL.7 This pattern of associations supports the construct validity of the K-BIS.
In further support of the discriminant validity of this instrument, women who underwent mastectomy scored significantly higher on the scale than those who underwent BCS or oncoplastic surgery. At first, One-way ANOVA was used to explore the differences between the BCS subgroup and Mastectomy subgroup. The ANOVA [F(1,106)=4.102, p=0.045] revealed that patients who were treated by mastectomy (M=10.17, SD=8.22) presented significantly more body image concerns than those treated by BCS (M=7.33, SD=6.26). This supports the utility of the K-BIS for differentiating surgery groups characterized by different appearance changes. This finding is in line with previous research and also with the results of the BIS study.24-27 We conducted the second analysis that covered the oncoplastic surgery subgroup. The ANOVA revealed that patients in the mastectomy subgroup presented significantly more body image concerns than the BSC subgroup or oncoplastic surgery subgroup. After the post hoc test, the statistical significance was shown to exist only between the mastectomy subgroup and oncoplastic surgery subgroup (p=0.017). At the last, we conducted the ANCOVA to control the differences of age and stage at surgery may affect the score of K-BIS. The ANCOVA revealed that the differences of age and stage at surgery didn't affect the K-BIS scores of patients (p=0.690, p=0.084). And there were statistically significant score differences of K-BIS among the subgroups, regardless of the differences of age and stage at surgery (p=0.007, p=0.035). This result is a new finding which has not been studied in previous BIS validation researches.
The present findings must be cautiously interpreted considering the following limitations. First, the absence of longitudinal data made the examination of the temporal stability of the scale impossible, which would add support for its reliability. Future longitudinal research is needed to examine the test-retest reliability of the K-BIS in a larger sample than 32 retest participants and also to further explore the influence of time since diagnosis on body image. Second, the study subjects were not recruited from the general cancer populations and included only breast cancer patients. Thus, generalizing results across the general cancer population would be difficult. Future research is also needed to confirm the unidimensionality and the psychometric performance of the BIS in other cancer populations.
In conclusion, the Korean version of the BIS (K-BIS) had good psychometric properties and can be used as a reliable and valid tool to assess the body image concerns on a sample of breast cancer patients. Its brevity and comprehensibility allow a rapid and clear assessment, both on clinical and research settings, complementing the QOL measurement of cancer patients when body image is considered an important outcome for them. This could be an important assessment tool for health care workers who work with cancer patients, as it provides a brief and clear assessment of body image issues of cancer patients. Further studies are needed to fully evaluate the K-BIS, including its application to other cancer populations.