1. Blazer D. Major depression in later life. Hosp Pract (Off Ed) 1989;24:69-76. 79PMID:
2777943.

2. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997;349:1436-1442. PMID:
9164317.


3. Sonnenberg CM, Beekman AT, Deeg DJ, Van Tilburg V. Drug treatment in depressed elderly in the Dutch community. Int J Geriatr Psychiatry 2003;18:99-104. PMID:
12571816.


4. Judd LL, Rapaport MH, Paulus MP, Brown JL. Subsyndromal symptomatic depression: a new mood disorder? J Clin Psychiatry 1994;55(Suppl):18-28. PMID:
8077164.

5. Wells KB, Burnam MA, Rogers W, Hays R, Camp P. The course of depression in adult outpatients. Results from the Medical Outcomes Study. Arch Gen Psychiatry 1992;49:788-794. PMID:
1417431.


6. Sherbourne CD, Wells KB, Hays RD, Rogers W, Burnam MA, Judd LL. Subthreshold depression and depressive disorder: clinical characteristics of general medical and mental health specialty outpatients. Am J Psychiatry 1994;151:1777-1784. PMID:
7977885.


7. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale a preliminary report. J Psychiatr Res 1982-1983;17:37-49. PMID:
7183759.

8. Beck AT. The Beck Depression Inventory. 1978,Philadelpia: Center for Cognitive Therapy.
9. Radloff LS. The CES-D scale: a report depression scale for research in general population. Apple Psychol Measurement 1977;1:385-401.

10. Zung WW. A self-rating depression scale. Arch Gen Psychiatry 1965;12:63-70. PMID:
14221692.


11. Kee BS, Kim SY. A preliminary study for the standardization of geriatric depression scale in Korea. J Korean Neuropsychiatr Assoc 1996;35:298-307.
12. Jung IK, Kwak DI, Shin DK, Lee MS, Lee HS, Kim JY. A reliability and validity study of Geriatric Depression Scale. J Korean Neuropsychiatr Assoc 1997;36:103-112.
13. Cho MJ, Bae JN, Suh GH, Hahm BJ, Kim JK, Lee DW, et al. Validation of Geriatric Depression Scale, Korean Version (GDS) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc 1999;38:48-63.
14. Kim JM, Shin IS, Yoon JS, Lee HY. Validity of Korean form of Geriatric Depression Scale according to cognitive function in a community dwelling elderly population. Kor J Psychopathol 2001;10:126-131.
15. Wancata J, Alexandrowicz R, Marquart B, Weiss M, Friedrich F. The criterion validity of the Geriatric Depression Scale: a systematic review. Acta Psychiatr Scand 2006;114:398-410. PMID:
17087788.


16. Park JH, Lim S, Lim JY, Kim KI, Yoon IY, Kim JM, et al. An overview of the Korean Longitudinal Study on Health and Aging. Psychiatry Invest 2007;4:84-95.
17. Lee DY, Lee KU, Lee JH, Kim KW, Jhoo JH, Youn JC, et al. A normative study of the Mini-Mental State Examination in the Korean elderly. J Korean Neuropsychiatr Assoc 2002;41:508-525.
18. Lee JH, Lee KU, Lee DY, Kim KW, Jhoo JH, Kim JH, et al. Development of the Korean version of the Consortium to Establish a Registry for Alzheimer's Disease Assessment Packet (CERAD-K): clinical and neuropsychological assessment batteries. J Gerontol B Psychol Sci Soc Sci 2002;57:P47-P53. PMID:
11773223.



19. Association AP. Diagnostic and statistical manual of mental disorders. 2000,Washington D.C.: American Psychiatric Association.
20. Cho MJ, Kim KH. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc 1993;32:381-399.
21. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62. PMID:
14399272.



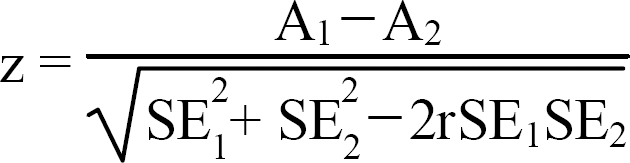
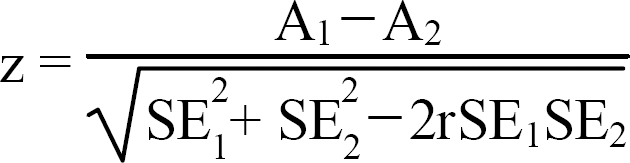
22. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983;148:839-843. PMID:
6878708.



23. Sheikh JI, Yesavage JA, Brooks JO 3rd, Friedman L, Gratzinger P, Hill RD, et al. Proposed factor structure of the Geriatric Depression Scale. Int Psychogeriatr 1991;3:23-28. PMID:
1863703.


24. Ryu KH, Kang YW, Na DL, Lee KH, Chung CS. The characteristics of Depression in Dementia Patients. Kor J Clin Psychol 2000;19:117-129.
25. Adams KB. Depressive symptoms, depletion, or developmental change? Withdrawal, apathy, and lack of vigor in the Geriatric Depression Scale. Gerontologist 2001;41:768-777. PMID:
11723345.