 |
 |
- Search
| Psychiatry Investig > Volume 15(6); 2018 > Article |
|
Abstract
Objective
This study is a prospective observational study on 75 late-adolescent survivors of a large passenger ship accident from immediately after the accident to one year later.
Methods
Assessments of student survivors were conducted on day 2 and at months 1, 6, and 12. The PTSD Checklist (PCL), Patient Health Questionnaire-9 (PHQ-9), State subscale of the State and Trait Anxiety Inventory (STAI-S), Athens Insomnia Scale (AIS), and Brief Resilience Scale (BRS) were administered.
Results
When the assessments for day 2 and month 12 were compared, all the scales, except the PCL-avoidance subscale, showed a significant improvement in symptoms among males. However, among females, all the scales, except the PCL-re-experience subscale and the STAI-S, failed to show a significant improvement. All the symptoms for both males and females showed a pattern that decreased to the lowest level at month 1 (camp-based controlled intervention period), then increased at months 6 and 12 (voluntary individual treatment after returning to school).
A large passenger ship carrying 476 people sank in the Yellow Sea on April 16, 2014. Among the passengers were 325 high school sophomores on a school trip; 250 died or went missing, and only 75 were rescued. These 75 survivors lost their friends and teachers, and went through a difficult recovery process [1,2].
Adolescents exposed to disasters have different perspectives than adults and require meticulous care. Youth are more vulnerable to posttraumatic stress disorder (PTSD) than adults, and have a higher possibility of chronicization [3]. In addition, adolescents are sensitive to environmental changes in the local community and schools, and the influence from their peers and family is considerable [4]. Exposure to disasters in adolescence causes not only adaptational problems directly related to trauma, but also secondary sequelae, such as impulsive or aggressive behaviors, substance abuse, and academic failure [5]. These sequelae interrupt the normal development of adolescents, continuing to impact on their development into adulthood [6].
Among several age groups of children and adolescents, disaster intervention in late adolescence generally has two conflict perspectives. First, like children, late adolescents have low levels of awareness about the help that they need; even if they recognize that they need help, they do not want to express their difficulties and have a tendency not to ask for external assistance [7]. Therefore, it is recommended that a controlled environment is created through a community or school-based intervention [8,9]. Second, late adolescents have mindsets and identities close to those of adults. Therefore, they have a high demand for autonomy and independence [10]. In fact, this age group may show similar symptoms of posttraumatic stress and prognosis as adults [11]. Therefore, although they are still minors, an adolescent strongly opposes being considered someone who needs the consent and protection of their guardians or specialists. If treatment is forced onto this late adolescent group, there may be backlash and resistance. Therefore, controlled intervention for a reasonable period is recommended, rather than a long-term obligatory intervention. Thus, unforced autonomous counseling and interventions are quite effective [12].
This study was conducted to investigate the changes in the symptoms and recovery process from an accident to one year later among late-adolescent survivors of the same age, who attended the same school, and who lived in the same area. The main hypotheses of this study were as follows: First, because of previous studies on adolescents [13], various psychiatric symptoms, including posttraumatic stress symptoms, would improve considerably one year after the accident. Second, the changes in symptoms might be associated with the environment of the controlled group treatment (up to week 10) and that of the voluntary individual treatment (after week 10). Finally, considering that the student survivors were in late adolescence, there might be differences caused by gender. The ultimate goal of this study was to gain insights that could help support adolescent victims of disasters and to examine changes in survivors’ symptoms.
The study participants were 75 student survivors of a ferry accident. All the survivors were rescued from the same ship on the same day. All were sophomore students aged 17, with 34 males and 41 females. All the student survivors were enrolled in the same school (Danwon High School) and living in the same city (Ansan).
On the day they were rescued, the students were transferred to a university hospital, where they underwent inpatient treatment for two weeks. During this period, physical and psychological examinations were conducted, and controlled group treatment and individual counseling were provided. After two weeks of inpatient treatment, 71 students were discharged, and four students with serious symptoms remained hospitalized. The school, Office of Education, and parents thought that it would be impossible for the discharged student survivors to immediately go back to their daily routines or return to school. Therefore, the student survivors were sent to a training institute and stayed in a camp for 8 weeks where they underwent a group treatment program and took classes. Students were allowed to spend enough time with their families at the camp if they wanted. Thereafter, all the student survivors returned to their respective homes and school. They were assigned new classrooms, classes, and homeroom teachers, and a counseling center was opened inside the school. The students received follow-up observation and voluntary individual treatment at any of the two locations (or both if desired): a psychiatric outpatient clinic at the university hospital, where they first received inpatient treatment, or a counseling center inside the school. The hospital had one psychiatrist exclusively responsible for the student survivors, and five other psychiatrists. The counseling center had one psychiatrist and several psychologists. The students used the hospital or school counseling center for free; the costs of the treatment and counseling were fully covered by the government.
A hospital and a school were chosen as the treatment locations, as the counseling center inside the school was familiar to the students and was very accessible, while the hospital could easily conduct physical and psychological examinations. If the students wanted counseling confidentiality, the hospital was advantageous to meet this need.
This was a 1-year prospective observational study without specific therapeutic manipulation that followed the natural course of symptoms of the student survivors. All the student survivors were evaluated for mental status by psychiatrists on day 2 and at months 1, 6, and 12. At these time points, the students who consented to this study completed self-report questionnaires that were designed to measure posttraumatic stress, depression, and anxiety symptoms, as well as their sleep patterns and degree of resilience after the disaster. Examinations were conducted on day 2, when the student survivors were admitted to the hospital, and were conducted in the camp at month 1. At months 6 and 12, the students visited the hospital and were examined. All the subjects provided written informed consent. This study was approved by the Institutional Review Board of Korea University Ansan Hospital (2014AS0290).
The PCL is a self-report measure suitable for screening for PTSD and documenting changes in its symptoms [14]. It was developed in 1991 based on the Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R and then revised according to the DSM-IV in 1993. Recently, the DSM-5 version was developed. We used the DSM-IV based PCL to easily compare our results with those from previous studies. The PCL has 17 items, and respondents rate their individual symptoms for the past month on a scale from 1-5. The PCL has three subscales: re-experience (5 items), avoidance (7 items), and hyperarousal (5 items). The PCL is commonly used when a clinical interview is not feasible [15], and is regularly used with adolescents [16]. A cut-off score of 50 is widely used to classify an adolescent as having PTSD [15,17].
PHQ-9 is a self-report depression assessment tool consisting of nine items and is designed to be consistent with the diagnostic evaluation of a depressive episode in the DSM-IV [18]. The cut-off score for screening for a major depressive disorder in the 13-17 age group is 11 [19]. The scores of this questionnaire are scored with a four point scale (0-3 points), yielding a total score of 27. The last item, question 9, assesses the degree of suicidal ideation of the respondent.
This self-report tool was developed to measure temperamental anxiety (trait) and current subjective anxiety (state), and is scored with a four point scale (1-4 points) [20]. This study used only the STAI state form, with 20 questions for analysis to measure the present level of anxiety of the respondent.
This is a self-report questionnaire quantifying sleep difficulty based on the ICD-10 diagnostic criteria for insomnia and is scored with a four point scale (0-3 points) [21]. Of the eight questions, the first five assess sleep induction, awakenings during the night, final awakening, total sleep duration, and sleep quality, respectively. The next three questions assess the respondent’s well-being, functional capacity, and sleepiness during the day.
This self-report measure consists of six questions, three of which are positive, and three negative [22]. Each question is assigned a score from 1-5, and the scores of the negative questions are summed inversely. A higher total score reflects a higher degree of resilience.
Missing data were replaced with the median of the complete data for each item. The number of missing values for each item was less than 1.0%. The descriptive statistics for each variable were calculated. Frequencies of categorical data were analyzed using chi-square or Fisher’s exact tests. Subjects with PTSD were defined as those with a PCL total score of 50 or higher. It is known that posttraumatic stress, depression, and anxiety symptoms may differ by gender among adults [23]. As the participants were in late adolescence, the analysis was stratified by gender.
The total scores on the PCL, its three subscales (re-experience, avoidance, and hyperarousal), PHQ-9, STAI-S, AIS, and BRS in each gender group were calculated separately for four time points (day 2 and months 1, 6, and 12) after the accident. The BRS was not measured on day 2 but was starting at month 1. The differences in these total scores after the four time points were assessed by two-factor analysis of variance (ANOVA) for each gender and time point. The differences were compared using Bonferroni post-hoc tests between the periods. If the score for the last (9th) item of the PHQ was 0, there was considered to be no suicidal ideation. If it was 1 or higher, it was considered that there was suicidal ideation.
A power analysis were conducted for all analyses. In all tests, a significance level of p<0.05 was used. All analyses were conducted using Statistical Package for the Social Sciences for Windows, version 20.0 (IBM Corp., Armonk, NY, USA).
Table 1 summarizes the group, individual, family, and social therapies administered at each period of hospital-based controlled (0-2 weeks), camp-based controlled (3-8 weeks), and school-based voluntary (after 3 months) intervention. Among the students who received individual treatment in the period of school-based voluntary intervention, one participant received repetitive transcranial magnetic stimulation (15 sessions), four received eye movement desensitization and reprocessing (mean of eight sessions), and five received individual trauma-focused-cognitive behavior therapy (mean of 10 sessions).
Subjects who completed the regular psychological assessments were designated as “completers.” Non-completer rate was high at month 6 (26.7%). However, the total scores of PCL, PHQ-9, STAI-S, and AIS on day 2 between the completer and non-completer at month 6 were not statistically significant. The total scores of those scales at month 1 between completer and non-completer at month 6 also showed no statistically differences. There was no difference in the proportion of males and females who did not complete the measures in each period (Table 2).
Although there were no male subjects with PTSD at month 1, there were two (8.0%) at month 6, and two (6.5%) at month 12. Females reported more PTSD compared to males, with six (15.0%, 20.0%, 16.7%) subjects at months 1, 6, and 12, respectively (month 1; χ2=5.70; df=1; p=0.027). At all time periods, there were more female subjects for whom psychotropic medicines were prescribed than male subjects (month 1; χ2=4.20; df=1; p=0.040). The proportion of female subjects who visited the hospital or the counseling center in the school was higher than that of male subjects at all time periods (month 12; χ2=7.17; df=1; p=0.007).
The total PCL scores by time period were first compared and then stratified by gender (Table 3, Figure 1). Among all subjects, the PCL scores at month 1 significantly decreased compared to day 2 (day 2 vs. month 1: p<0.001). Total PCL scores, however, significantly increased at months 6 and 12 (month 1 vs. month 6: p<0.05; month 1 vs. month 12: p<0.01); the average total PCL score increased to the severity level at 2 day. In general, there were no significant changes in the total PCL scores over time (time: F=4.98; not significant).
There were significant differences in total PCL scores between male and female subjects over time (time×gender: F=4.23; p=0.013). Among males, total PCL scores significantly decreased at month 1 compared to day 2 (day 2 vs. month 1: p<0.01). Although scores slightly increased at months 6 and 12, they were still significantly lower than those on day 2 (day 2 vs. month 6: p<0.05; day 2 vs. month 12: p<0.05). Among females, the total PCL scores significantly decreased at month 1 compared to day 2 (day 2 vs. month 1: p<0.05). These scores started increasing, however, at months 6 and 12 (month 1 vs. month 12: p<0.01), and total PCL scores at month 12 were slightly higher than those on day 2.
Table 3 and Figure 1 show changes in the PCL subscales total scores by time period for the assessment completers, and stratified by gender. In the completers, significant changes in scores over time were seen in the re-experience subscale (time: F=8.04; p<0.0001). A significant difference between male and female subjects over time was seen in the re-experience subscale (time×gender: F=2.12; p=0.045) and the avoidance subscale (time×gender: F=2.87; p=0.001).
In the re-experience subscale, the total score of the male subjects significantly decreased at month 1 (day 2 vs. month 1: p<0.001) and these reductions remained significant at months 6 and 12 (day 2 vs. month 6: p<0.001; day 2 vs. month 12: p<0.001). Finally, the total score was lowest at month 12 (month 1 vs. month 12: p<0.05; month 6 vs. month 12: p<0.01). Among female subjects, the total score significantly decreased at month 1 (day 2 vs. month 1: p<0.05), increased at month 6, then decreased again at month 12. Finally, the difference in total score between day 2 and month 12 was statistically significant (day 2 vs. month 12: p<0.05).
In the avoidance subscale, the total scores of the male subjects significantly decreased at month 1 (day 2 vs. month 1: p<0.01), then significantly increased at months 6 and 12 (month 1 vs. month 6: p<0.05; month 1 vs. month 12: p<0.05), with scores at month 12 similar to the scores on day 2. The total scores of the female subjects did not decrease at month 1, then greatly increased at months 6 and 12, ending up significantly higher than the scores on day 2 (day 2 vs. month 6: p<0.01; day 2 vs. month 12: p<0.01; month 1 vs. month 6: p<0.01; month 1 vs. month 12: p<0.01).
In the hyperarousal subscale, the total scores of the male subjects greatly decreased at month 1 and were maintained until month 6 (day 2 vs. month 1: p<0.001; day 2 vs. month 6: p<0.001). While hyperarousal scores significantly increased at month 12 (month 1 vs. month 12: p<0.01; month 6 vs. month 12: p<0.01), they remained significantly lower than those of day 2 (day 2 vs. month 12: p<0.05). The total scores for the female subjects significantly decreased at month 1 (day 2 vs. month 1: p<0.05) then significantly increased from month 6 to month 12 (month 1 vs. month 12: p<0.01; month 6 vs. month 12: p<0.05), ending up slightly higher than hyperarousal scores on day 2.
Table 4 and Figure 2 show the changes in the PHQ-9, STAI-S, and AIS total scores at each time period for the assessment completers, as well as the sample stratified by gender. In the completers, the changes in scores over time were significant for the PHQ-9 (time: F=7.23; p<0.0001), the STAI-S (time: F=19.76; p<0.0001), and the AIS (time: F=10.62; p<0.0001). A significant difference between the male and female subjects over time was found in PHQ-9 scores (time×gender: F=5.77; p=0.001).
In the PHQ-9, the total scores of the male subjects decreased greatly at month 1 (day 2 vs. month 1: p<0.001), and these reductions remained significant at months 6 and 12 (day 2 vs. month 6: p<0.01; day 2 vs. month 12: p<0.05). For the female subjects, there was no decrease in the PHQ-9 total scores at months 1 and 6. However, the scores significantly increased at month 12 (month 6 vs. month 12: p<0.01), and were slightly higher than the scores on day 2.
In the STAI-S, the total scores of the male subjects decreased greatly at month 1 (day 2 vs. month 1: p<0.001). These reductions remained significant at month 6 (day 2 vs. month 6: p<0.001). Although they increased slightly from month 6 to 12, the total score at month 12 was still significantly lower than the score on day 2 (day 2 vs. month 12: p<0.05). The total scores of the female subjects decreased greatly at month 1 (day 2 vs. month 1: p<0.001), and maintained their decreased status at months 6 and 12 (day 2 vs. month 6: p<0.001; day 2 vs. month 12: p<0.001).
The AIS total scores of the male subjects decreased greatly at month 1 (day 2 vs. month 1: p<0.001), and these reductions remained significant at months 6 and 12 (day 2 vs. month 6: p<0.01; day 2 vs. month 12: p<0.01). In contrast, the AIS scores of the female subjects significantly decreased at month 1 (day 2 vs. month 1: p<0.01) then increased from month 6, such that there was no significant difference in AIS total score between day 2 and month 12.
Table 2 presents the number of subjects with a score of 1 or higher on the suicidal ideation assessment, the last item of the PHQ-9. The number of subjects with suicidal ideation included 4 males and 15 females on day 2 (χ2=7.06; p=0.009), 1 male and 8 females at month 1 (χ2=5.38; p=0.030), 2 males and 5 females at month 6, and 1 male and 10 females at month 12 (χ2=6.17; p=0.017). The proportion of females with suicidal ideation was higher at every time period.
Table 4 and Figure 2 present the BRS total scores at every time period for the completers and for the sample stratified by gender. In the completers, total scores significantly decreased over time, indicating that resilience was decreasing (time: F=12.27; p<0.0001). There were significant gender differences over time (time×gender: F=7.12; p=0.006). While the BRS total scores of the male subjects significantly decreased at month 6 compared to month 1 (month 1 vs. month 6: p<0.001) and maintained their decreased status at month 12 (month 1 vs. month 6: p<0.001), there were no significant decreases in the total scores of the female subjects at months 6 and 12 compared to month 1.
The study subjects had different characteristics in their recovery environment compared with subjects of previous studies of youth disasters. All subjects of this study were in late adolescence, were the same age, belonged to the same school, and suffered through an accident while on a school trip.
To minimize the psychological damage incurred by the adolescents from the trauma they experienced, resources from the school, community, and healthcare institution were sent immediately after the disaster so that the utmost assistance could be provided to the survivors [1,2]. In contrast to our first hypothesis, however, there was no significant improvement in the posttraumatic stress symptoms of the completers after 12 months. The main reason for this is that there was almost no improvement in the symptoms of the female survivors. Another reason is that the total observation period for the changes in the symptoms was 12 months, which might have been an insufficient amount of time. Many studies have reported that the PTSD of children and adolescents can last longer than that of adults and that PTSD can be prolonged for several years after a disaster [24]. Meanwhile, the prevalence of PTSD during the first year after the accident was 0% to 8.0% for males and 15% to 20% for females. This suggests that there were many survivors who had subsyndromal levels of PTSD. Therefore, there were only a few of the study subjects who have experienced substantially decreased PCL total scores.
It was theorized that the reasons for the lack of improvement in posttraumatic stress symptoms among female subjects compared to male subjects were as follows. First, it may be because female adolescents are much more vulnerable to depression and anxiety disorders than are male adolescents, and anxiety disorders are more common in females across the lifespan [25]. Considering depression, gender differences appear at 13-15 years old, rapidly increase in female adolescents, then remain persistent in adults [26]. This vulnerability to depression and anxiety in female adolescents might interfere with recovery from posttraumatic stress symptoms.
Second, the measurement of depression, anxiety, and sleep conducted in this study may have over-presented the problems of the female adolescents. In many cases, adolescents show behavioral problems after a disaster, rather than posttraumatic stress symptoms related to the disaster [5]. These behavioral problems are broadly categorized into internalization (e.g., depression, anxiety) and externalization (e.g., aggressiveness, substance abuse, and delinquency). In general, female adolescents engage in more internalization, while male adolescents engage in more externalization [25].
Lastly, adolescents have different ways of responding to trauma depending on gender [27]. Female adolescents tend to share feelings of loss after trauma with family, friends, and therapists, and think highly of recommendations from these resources. The higher rate of voluntary visits to the treatment facilities by female subjects in the study supports this observation. Male adolescents, however, tend to think that their mental health is a function of their will or attitude, and rarely express their feelings. Therefore, male adolescents, like male adults, tend to underreport symptoms in self-report assessments [28]. In this study, even though the male adolescent subjects’ resilience significantly decreased at months 6 and 12 compared to month 1, they reported that their posttraumatic stress symptoms had improved.
Generally, after the acute phase of a disaster, people show a pattern in which the psychological symptoms of trauma stay the same or are slightly aggravated until the subacute phase, then gradually improve in the chronic phase [29]. In this study, however, all symptoms decreased to their lowest level at month 1 (subacute phase), lower than on day 2 (acute phase), then increased again at months 6 and 12 (chronic phase). This might have been the result of the controlled treatment, including hospitalization and camping. During this period, the survivors were protected from secondary trauma by preventing exposure to media, funerals, and memorial ceremonies, which minimized their acute stress responses, abnormal grief reactions, and guilty feelings. This was the period when the feelings of solidarity and the drive to conquer their trauma was motivated through group therapy. This means that the controlled and systematic rehabilitation efforts of the connected organizations of the school, the community, and the healthcare institution created a very critical recovery environment for the adolescents, who had limited knowledge of the types of help that they needed to ask for, and who had difficulty asking for external help.
The voluntary individual treatment period began in month 3 and resulted in the aggravation of various symptoms at the chronic phase (months 6 and 12). This aggravation of symptoms at the chronic phase may have been caused by a variety of factors.
Many studies reported that the school is the best place for students to recover from their psychological trauma after a disaster [30]. This disaster, however, occurred while the students were on a school trip and as such, the school itself became a disaster site. When the survivors came back to school in reorganized classes, coming to the school itself was like revisiting the disaster site. In addition, the fact that the previous classrooms were kept empty for a long time after the disaster, as they were made into a memorial site, might have had a negative impact on the student survivors’ trauma recovery.
The survivors might have reported aggravated symptoms at month 12 because that time coincided with the memorial period for the first anniversary of the accident. Furthermore, there was intense media coverage of the disaster on its first anniversary. Although the survivors went back to their respective daily routines and spent considerable amounts of time doing so, media reports about the accident continued, and the student survivors were repeatedly exposed to images of the sinking ferry or rescue scenes. The disaster circumstances that came to be recalled by the adolescent survivors caused changes in their posttraumatic stress response, and sustained their stress. Many studies reported the association between posttraumatic stress symptoms and exposure to TV in adolescents [31,32].
After a disaster, adolescents tend to observe the coping strategies and behavior of their parents or other adults in the disaster-affected area, and seek stability or imitate healthy behaviors [33]. Although this disaster was a local community disaster, the parents of the survivors and the other adults in the community did not experience the disaster all together. Therefore, the survivors may have perceived the absence of recovery role models among their parents and other adults. There were external factors during the chronic phase that lowered the adaptability of the survivors, such as problems with compensation for the accident, career paths, stress from upcoming entrance examinations, and socio-political situations that compromised the recovery environment [1,2]. Study subject characteristics and the distinct characteristics of this particular disaster might have been factors that resulted in sustained stress after the traumatic event (posttraumatic stress and adversity factors).
The limitations of this study and the further needed studies are as follows. The 12-month observation period may have been insufficient, and therefore, more long-term observation is needed. To accomplish this, our study team will conduct follow-up observations for several years. Second, adolescent assessment tools were not used to measure various youth problems, such as drinking, smoking, internet use, and behavioral problems, like delinquency, grief response, physical symptoms, and quality of life. Furthermore, positive changes, like posttraumatic growth [34], were not measured. Third, only quantitative research was conducted; qualitative research through in-depth interviews is also needed. Fourth, attachment to one’s parents, family functions, and childhood experiences are very important in adolescents’ recovery from trauma [33], but they were not investigated in this study. Fifth, the study subjects were not diagnosed based on structured clinical interviews, and the non-systemic and various psychological treatments are applied in some students. Sixth, the number of adolescent survivors who did not participate in the study was 1 (1.3%) on day 2 and at month 1, 20 (26.7%) at month 6 and 5 and (6.7%) at month 12. Most of the student survivors who did not participate in this study rarely visited the treatment center. It is necessary to find out why these students did not visit the treatment center-whether it is because they had fewer psychological problems than the rest of the students, or if they hesitated to visit because they were reluctant to get help or mental health counseling, or possibly these students were greatly affected by avoidance symptoms.
After the 12-month follow-up, many of the psychological symptoms experienced by the female adolescent subjects had not improved. Female adolescents are more sensitive to traumatic experiences than male adolescents, and their coping methods differ from those of male adolescents. Accordingly, much closer attention should be paid towards female adolescent disaster survivors. Although controlled school and community-based interventions were very effective for the survivors, such intensive interventions cannot be applied long-term. Therefore, this school and community-based intervention needs to be changed into a more autonomous treatment over time. All the symptoms for both males and females showed a pattern that decreased to the lowest level at month 1 (camp-based controlled intervention period), then increased at months 6 and 12 (voluntary individual treatment after returning to school). A rapid deterioration of psychological symptoms was found during chronic phase, when students returned to their daily routines. In the chronic phase, most of the psychological symptoms for females were at subsyndromal level, but were close to the level of initial deterioration. During the same period, many of the symptoms for males showed improvement, but resilience showed worsening. Therefore, it is very important to screen high-risk adolescent survivors and to show an intense interest in them during this period. Furthermore, this study needs to be continued for several years to follow up on the subjects’ symptoms, while supplementing its limitations.
ACKNOWLEDGEMENTS
This study was supported by the Jisan Cultural Neuropsychiatry Research Fund (2017) of the Korean Foundation of Neuropsychiatry Research.
Figure 1.
PCL total scores and PCL subscales total scores on day 2 and at months 1, 6, and 12. *p<0.05, vs. 2 days after, †p<0.01, vs. 2 days after, ‡p<0.001, vs. 2 days after, §p<0.05, vs. 1 month after, ǁp<0.01, vs. 1 month after, ¶p<0.05, vs. 6 month after, **p<0.01, vs. 6 months after. PCL: Posttraumatic Stress Disorder Checklist.
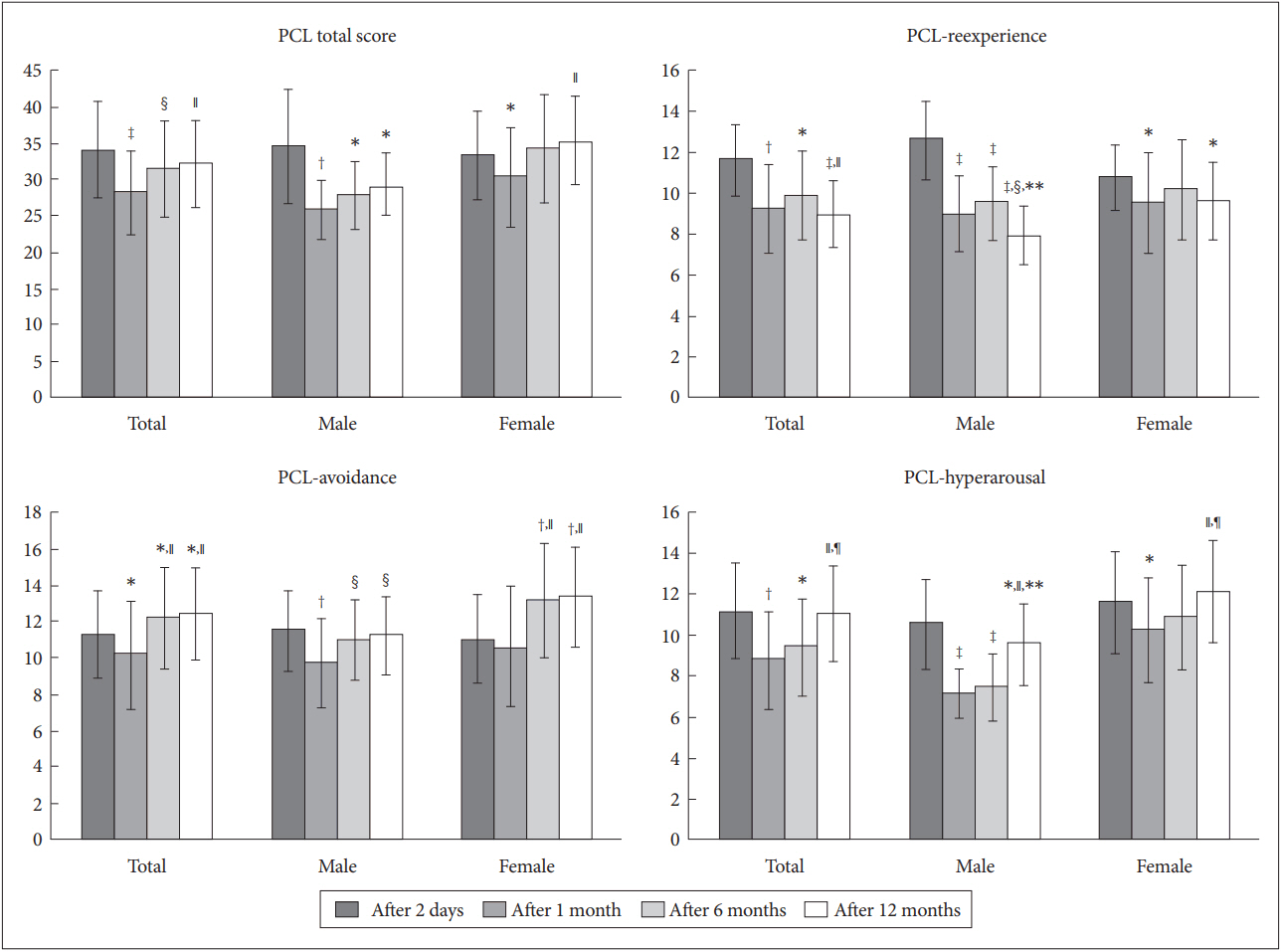
Figure 2.
Total scores in PHQ-9, STAI-S, AIS, and BRS on day 2 and at months 1, 6, and 12. *p<0.05, vs. 2 days after, †p<0.01, vs. 2 days after, ‡p<0.001, vs. 2 days after, §p<0.05, vs. 1 month after, ǁp<0.01, vs. 1 month after, ¶p<0.05, vs. 6 month after, **p<0.01, vs. 6 months after. PHQ-9: Patient Health Questionnaire-9, STAI-S: State subscale of the Spielberger State and Trait Anxiety Inventory, AIS: Athens Insomnia Scale, BRS: Brief Resilience Scale.
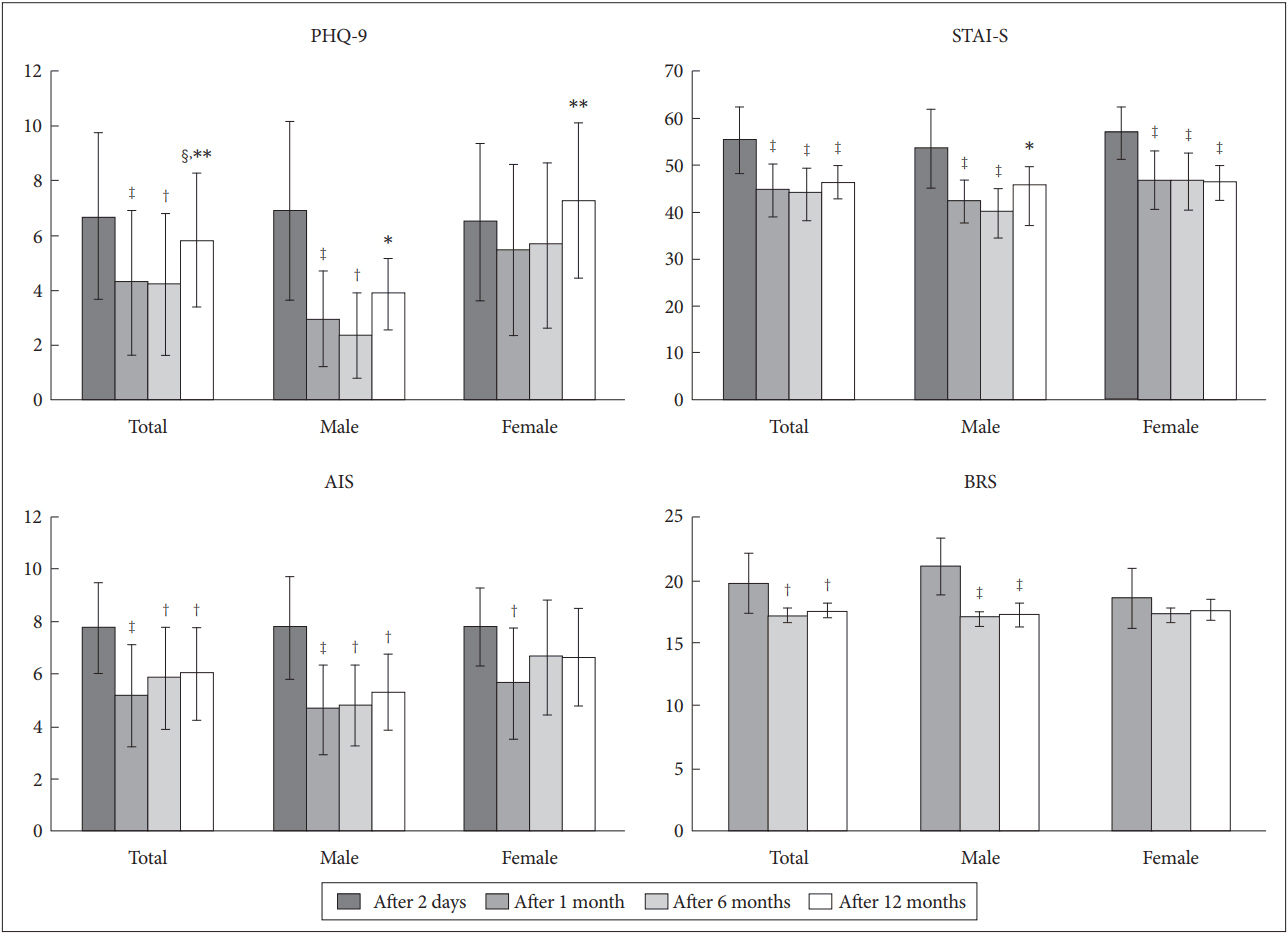
Table 1.
The group, individual, family, and social therapies administered at each period of hospital-, camp-, and school-based intervention
| Types of therapy | Hospital-based controlled intervention | Camp-based controlled intervention | School-based voluntary intervention |
|---|---|---|---|
| Period | 0-2 weeks (acute phase) | 3-8 weeks (subacute phase) | After 3 months (chronic phase) |
| Group therapy | Psychological first aid [35] | Skills for psychological recovery [36] | Cognitive behavioral intervention for-trauma in schools [38] |
| Mental health education | Group trauma-focused-CBT [37] | ||
| Mental health education | |||
| Individual therapy (N of subjects) | Supportive PT and PE | Supportive PT and PE | Supportive PT and PE |
| Interview for early detection-of risk group | Trauma-focused-CBT (5) | ||
| EMDR (4), rTMS (1) | |||
| Family or social therapy | PE (family) | Music therapy, art therapy, and-recreation (student and family) | Case management program in mental- health trauma center (family) |
| PE (family) | Teacher training program (school- teacher) |
Table 2.
Numbers of subjects who were treated with medications, visited the treatment facilities, and had PTSD or suicidal ideation on day 2 and at months 1, 6, and 12
|
Time period after disaster (T=75, M=34, F=41) |
|||||
|---|---|---|---|---|---|
| 2 days | 1 month | 6 months | 12 months | ||
| N of subjects prescribed psychotropic medication (%) | M | 6 (17.6) | 2 (5.9) | 3 (8.8) | 4 (11.8) |
| F | 13 (31.7) | 9 (22.0) | 10 (24.4) | 10 (24.4) | |
| Statistics | χ2=2.34 | χ2=4.20* | χ2=3.52 | χ2=2.27 | |
| N of subjects who visited the psychiatric outpatient (%) | M | 4 (11.8) | 5 (14.7) | ||
| F | 11 (26.8) | 17 (41.5) | |||
| Statistics | χ2=3.01 | χ2=7.17** | |||
| N of subjects who visited the counseling center in school (%) | M | 7 (20.6) | 12 (35.3) | ||
| F | 14 (34.1) | 21 (51.2) | |||
| Statistics | χ2=2.08 | χ2=2.51 | |||
| N of subjects who completed all assessments (%) | M | 34 (100) | 34 (100) | 25 (73.5) | 32 (94.1) |
| F | 40 (97.6) | 40 (97.6) | 30 (73.2) | 38 (92.7) | |
| T | 74 (98.7) | 74 (98.7) | 55 (73.3) | 70 (93.3) | |
| N of subjects with PTSD (%) | M | 0 (0) | 2 (8.0) | 2 (6.5) | |
| F | 6 (15.0) | 6 (20.0) | 6 (16.7) | ||
| Statistics | χ2=5.70* | χ2=1.69 | χ2=1.59 | ||
| N of subjects who had a suicidal ideation (%) | M | 4 (11.8) | 1 (2.9) | 2 (8.0) | 1 (3.2) |
| F | 15 (37.5) | 8 (20) | 5 (16.7) | 10 (27.8) | |
| Statistics | χ2=7.06** | χ2=5.38* | χ2=0.68 | χ2=6.17* | |
Table 3.
PCL total scores and PCL subscales total scores on day 2 and at months 1, 6, and 12
Table 4.
Total scores in PHQ-9, STAI-S, AIS, and BRS on day 2 and at months 1, 6, and 12
The number of subjects who complete all measures at each time point was shown in Table 2. T: total subjects, M: male subjects, F: female subjects, PHQ-9: Patient Health Questionnaire-9, STAI-S: State subscale of the Spielberger State and Trait Anxiety Inventory, AIS: Athens Insomnia Scale, BRS: Brief Resilience Scale, SD: standard deviation, NS: not statistically significant
REFERENCES
1. Woo H, Cho Y, Shim E, Lee K, Song G. Public trauma after the Sewol Ferry disaster: the role of social media in understanding the public mood. Int J Environ Res Public Health 2015;12:10974-10983.



2. Yang HJ, Cheong HK, Choi BY, Shin MH, Yim HW, Kim DH, et al. Community mental health status six months after the Sewol ferry disaster in Ansan, Korea. Epidemiol Health 2015;37:e2015046.




3. Pine DS, Cohen JA. Trauma in children and adolescents: risk and treatment of psychiatric sequelae. Biol Psychiatry 2002;51:519-531.


4. Cohen JA. Treating acute posttraumatic reactions in children and adolescents. Biol Psychiatry 2003;53:827-833.


5. Everstine DS, Everstine L. The Trauma Response: Treatment for Emotional Injury. New York: WW Norton & Co; 1993.
6. McDermott BM, Palmer LJ. Postdisaster emotional distress, depression and event-related variables: findings across child and adolescent developmental stages. Aust N Z J Psychiatry 2002;36:754-761.


7. Margolin G, Vickerman KA. Post-traumatic stress in children and adolescents exposed to family violence: I. Overview and issues. Prof Psychol Res Pr 2007;38:613-619.



8. Goenjian AK, Karayan I, Pynoos RS, Minassian D, Najarian LM, Steinberg AM, et al. Outcome of psychotherapy among early adolescents after trauma. Am J Psychiatry 1997;154:536-542.


9. Pynoos RS, Goenjian AK, Steinberg AM. A public mental health approach to the postdisaster treatment of children and adolescents. Child Adolesc Psychiatr Clin N Am 1998;7:195-210.


10. Frank SJ, Pirsch LA, Wright VC. Late adolescents’ perceptions of their relationships with their parents: relationships among deidealization, autonomy, relatedness, and insecurity and implications for adolescent adjustment and ego identity status. J Youth Adolesc 1990;19:571-588.



11. Yule W, Bolton D, Udwin O, Boyle S, O’Ryan D, Nurrish J. The long-term psychological effects of a disaster experienced in adolescence: I: The incidence and course of PTSD. J Child Psychol Psychiatry 2000;41:503-511.


12. Allen JP, Kuperminc G, Philliber S, Herre K. Programmatic prevention of adolescent problem behaviors: the role of autonomy, relatedness, and volunteer service in the Teen Outreach Program. Am J Community Psychol 1994;22:617-638.


13. Becker DF, Weine SM, Vojvoda D, McGlashan TH. Case series: PTSD symptoms in adolescent survivors of “ethnic cleansing.” Results from a 1-year follow-up study. J Am Acad Child Adolesc Psychiatry 1999;38:775-781.


14. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996;34:669-673.


15. Jia Z, Tian W, Liu W, Cao Y, Yan J, Shun Z. Are the elderly more vulnerable to psychological impact of natural disaster? A population-based survey of adult survivors of the 2008 Sichuan earthquake. BMC Public Health 2010;10:172




16. Cuffe SP, Addy CL, Garrison CZ, Waller JL, Jackson KL, McKeown RE, et al. Prevalence of PTSD in a community sample of older adolescents. J Am Acad Child Adolesc Psychiatry 1998;37:147-154.


17. Liu ZY, Yang YF, Ye YL, Zeng ZQ, Xiang YJ, Yuan P. One-year follow-up study of post-traumatic stress disorder among adolescents following the Wen-Chuan earthquake in China. Biosci Trends 2010;4:96-102.

18. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-613.



19. Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics 2010;126:1117-1123.



20. Spielberger CD. State-Trait Anxiety Inventory. New York: John Wiley & Sons; 2010.
21. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res 2000;48:555-560.


22. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15:194-200.


23. Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull 2006;132:959-992.



24. Green BL, Korol M, Grace MC, Vary MG, Leonard AC, Gleser GC, et al. Children and disaster: age, gender, and parental effects on PTSD symptoms. J Am Acad Child Adolesc Psychiatry 1991;30:945-951.


25. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol 1993;102:133-144.



26. Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol 1998;107:128-140.



27. Nada-Raja S, McGee R, Williams S. Health beliefs among New Zealand adolescents. J Paediatr Child Health 1994;30:523-529.


28. Gross JJ, John OP. Mapping the domain of expressivity: multimethod evidence for a hierarchical model. J Pers Soc Psychol 1998;74:170-191.



29. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med 2008;38:467-480.


30. Kataoka SH, Nadeem E, Wong M, Langley AK, Jaycox LH, Stein BD, et al. Improving disaster mental health care in schools: a community-partnered approach. Am J Prev Med 2009;37:225-229.

31. Nader KO, Pynoos RS, Fairbanks LA, al-Ajeel M, al-Asfour A. A preliminary study of PTSD and grief among the children of Kuwait following the Gulf crisis. Br J Clin Psychol 1993;32:407-416.


32. Pfefferbaum B, Moore VL, McDonald NB, Maynard BT, Gurwitch RH, Nixon SJ. The role of exposure in posttraumatic stress in youths following the 1995 bombing. J Okla State Med Assoc 1999;92:164-167.

33. Bokszczanin A. Parental support, family conflict, and overprotectiveness: predicting PTSD symptom levels of adolescents 28 months after a natural disaster. Anxiety Stress Coping 2008;21:325-335.


34. Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9:455-471.


35. Shaw JA, Espinel Z, Shultz JM. Care of Children Exposed to the Traumatic Effects of Disaster. 1st edition. Washington, DC: American Psychiatric Pub; 2012.
36. Berkowitz S, Bryant R, Brymer M, Hamblen J, Jacobs A, Layne C, et al. The National Center for PTSD & the National Child Traumatic Stress Network, Skills for Psychological Recovery: Field Operations Guide. 1st edition. Washington, DC and London: American Psychiatric Pub; 2010.






