INTRODUCTION
Trichotillomania is a frequently overlooked psychiatric condition characterized by repeatedly pulling out oneŌĆÖs own hair [1]. Despite being documented in the medical literature for almost two centuries, trichotillomania is poorly understood with limited data regarding its pathophysiological basis [2]. The symptoms in trichotillomania are overt and can be regarded as excessive grooming, a type of maladaptive behavior that is also observable in other species [3].
Oxidative stress results from the accrual of free radicals within the body. There is emerging data to suggest that oxidative stress may be involved in the pathophysiology of body focused repetitive behaviors such as trichotillomania. For example, in trichotillomania, the amino-acid n-acetyl cysteine (NAC) showed treatment efficacy versus placebo in a randomized, controlled trial, in adults [4], although a trial in children was negative [5]. NAC has also shown efficacy in skin picking disorder, in a randomized controlled trial, in adults [6]. NAC has effects on glutamatergic transmission in models of addiction [7,8] but also has antioxidative properties, raising the prospect of two potential underlying treatment mechanisms [9]. It is not known whether antioxidant, glutamatergic, or both mechanisms were important in mediating positive effects on trichotillomania symptoms in the adult treatment trial. A putative animal model of trichotillomania is the spontaneously occurring ŌĆśbarbering mouseŌĆÖ model, in which rodents excessively groom their cage mates, and to a lesser extent themselves [10]. Barbering mice have been reported to have elevated urinary antioxidant capacity, which the authors suggested was consistent with elevated oxidative stress in the animals associated with excessive grooming [11].
In view of the lack of studies examining compounds that may be influenced by oxidative stress in patients with trichotillomania, we measured a range of such compounds in a well-characterized sample of patients. We hypothesized that measures of oxidative stress would be abnormal in patients with trichotillomania and significantly correlate with more severe symptoms.
Methods
Subjects
Data from 14 participants with a primary diagnosis of trichotillomania were included in this study. Study procedures were carried out in accordance with the Declaration of Helsinki. The Institutional Review Board at the University of Chicago approved the study (FP059766-01-PR) and subjects provided written informed consent.
All subjects had a current DSM-5 primary diagnosis of trichotillomania. Other inclusion criteria included age 18 to 60 years, the ability to be interviewed in person, and willingness to provide a blood sample. Exclusion criteria included prior/current diagnosis of bipolar disorder, psychosis, or current substance use disorder. Current use of medication was not an exclusion criterion. No participant had previously used or currently was using NAC or any other antioxidant.
Assessments
Individuals were examined using a semi-structured interview by a board certified psychiatrist, enquiring about any history of mental disorders as well as current diagnostic criteria for trichotillomania. The interview included the Mini International Neuropsychiatric Inventory (MINI), which identifies conditions including mood, anxiety, and eating disorders [12].
Participants provided a blood sample, and plasma levels of the following compounds that may be influenced by oxidative stress were quantified: glutathione, angiotensin II, ferritin, iron, glucose, insulin and insulin growth factor 1 (IGF1), and hepcidin. Normative reference ranges were supplied by the analyzing laboratory. Choice of compounds was based on the literature examining NAC, grooming in animals, and general stress response [5,11,13].
Severity of trichotillomania, psychosocial dysfunction, and impulsivity were assessed with the following measures:
The Massachusetts General Hospital Hair Pulling Scale (MGH-HPS) [14,15]
The MGH-HPS is a valid and reliable seven-item, self-report scale that rates urges to pull hair, actual amount of pulling, perceived control over behavior, and distress associated with hair pulling over the preceding seven days.
Sheehan Disability Scale (SDS) [16]
The SDS is a valid and reliable scale that evaluates psychosocial dysfunction in three domains: work/school, social life, and home/family life.
Barratt Impulsiveness Scale, Version 11 (BIS-11)
The BIS-11 is a 30-item measure designed to assess impulsivity across three dimensions: attentional (inability to concentrate), motor (acting without thinking), and non-planning (lack of future orientation) [17]. BIS-11 was collected only for a subset (50%) of the sample.
Data analysis
Demographic, clinical, and oxidative stress data are presented in summary form. The number (%) of oxidative stress markers outside the normative reference ranges were summarized and compared against the null distribution using FisherŌĆÖs test. Relationships between oxidative stress marker levels and other measures (symptom severity, disability, and motor impulsiveness on the BIS-11) were examined using SpearmanŌĆÖs r. Statistical significance was defined as p<0.05 two-tailed. We did not adjust for multiple comparisons due to the exploratory nature of this study and sample size.
Results
The sample comprised 14 participants with trichotillomania [mean age of 31.2 (┬▒SD 8.8) years; 92.9% female]. The mean total score on the MGH-HPS was 16.6 (┬▒3.4) reflective of moderate symptom severity. Four participants had comorbid depression, and four had an anxiety disorder. One person reported a lifetime diagnosis of attention deficit hyperactivity disorder (ADHD). No other comorbidities were identified. Four patients (28.6%) were taking one or more psychotropic medications: fluoxetine 20 mg/day; citalopram 20 mg/day; escitalopram 20 mg/day; and fluoxetine 40 mg/day plus Adderall XL 30 mg/day. Levels of oxidative stress markers are summarized in Table 1. The proportion of participants with glutathione levels below the reference range (35.7%; n=5) differed significantly from the distribution expected under the null hypothesis by FisherŌĆÖs exact test (p=0.041). No other significant differences from the null hypothesis were detected for the other oxidative stress markers, in terms of proportions out of reference range (all p>0.10).
Average glutathione levels were 615.5 (131.30) uM in medicated cases, and 652.2 (SD 251.3) uM in the un-medicated cases. Average glutathione levels were 529.0 (219.0) uM in people with comorbid depression, and 674.5 (214.9) nM in those without; and were 680.0 (292.4) uM in people with comorbid anxiety disorder and 624.6 (192.1) uM in those without. These differences between subgroups of patients were not significant (all p>0.30 by WilcoxonŌĆÖs Z).
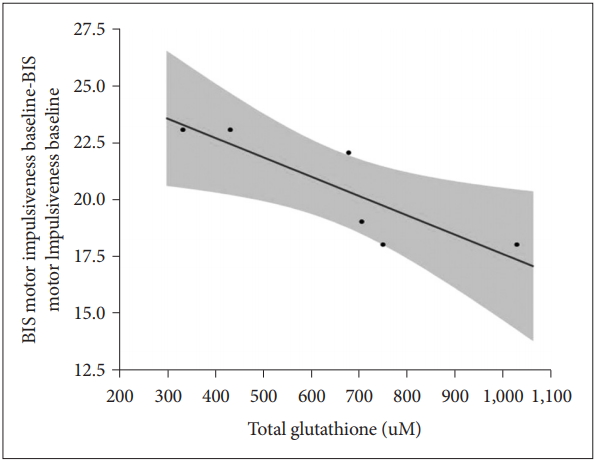
Lower levels of glutathione correlated highly significantly with higher motor impulsiveness on the BIS-11 in the 6 participants who completed the BIS-11 (r=0.97, p=0.001) (Figure 1). No other correlations between oxidative markers and BIS scores were significant (all p>0.05). Oxidative stress markers did not correlate significantly with symptom severity (MGH total scores) or disability (Sheehan Disability scores) (all p>0.10).
Discussion
The current study examined a range of blood oxidative stress markers in patients with trichotillomania. The key finding was that a significant proportion of patients had blood levels of glutathione that were below the external normative reference range. Furthermore, in a subset of the sample for whom Barratt Impulsiveness Scale scores were collected, lower levels of glutathione correlated significantly with higher motor impulsivity.
Glutathione is an antioxidant that eliminates free radicals. Oxidative stress pathways are increasingly implicated in a range of mental disorders but have received limited research attention. For example, reduced levels of glutathione have recently been reported in schizophrenia and bipolar disorder [18]. The current findings may partly explain why n-acetyl cysteine (NAC) shows efficacy in the treatment of trichotillomania and related disorders in some studies [4,6]. NAC is a cysteine precursor, and cysteine is the rate limiting step in the bodyŌĆÖs synthesis of glutathione [19]. Glutathione in turn is one of the major antioxidants within the body. It is important to note that NAC also has direct effects on the brainŌĆÖs glutamatergic pathways [9], and so not all its therapeutic actions necessarily stem from antioxidant effects.
Although there are no prior studies of oxidative stress in trichotillomania, some but not all studies have reported elevated oxidative stress markers in obsessive compulsive disorder (OCD). In an animal model of OCD characterized by stereotypic movements (deer mouse), evidence of deficient glutathione system was found in the cortex selectively [20]. One study of humans with OCD found lower glutathione levels in the posterior cingulate cortex [21], while another study found no significant differences in the total antioxidant status, total oxidant status and oxidative stress index levels between the OCD patients and control group, but serum 8-hydroxideoxiguanosine (8-OHdG) levels were significantly higher in OCD patients than controls [22]. Taken together with our results, these studies suggest that oxidative stress may be present in a sub-group of people with obsessive-compulsive related disorder such as trichotillomania. Although only a hypothesis, this in turn may also explain why an intervention such as NAC does not work in all people with trichotillomania. One could query whether only those with low baseline glutathione levels would respond to NAC. This also possibly explain the negative findings in the study of NAC in children with trichotillomania [5], as perhaps only a small percentage of those children had low levels of glutathione.
Although these findings are provocative, several limitations need to be considered. The study did not include an internal control group, and so identification of out-of-reference range measures relied on external norms, which are drawn from other population samples. However, external norms do have the advantage that they are independent of the current study and typically involve large sample sizes. The sample size was relatively small; as such, findings merit confirmation in a larger sample of patients in future. Causation cannot be confirmed in the absence of follow-up studies such as longitudinal examination. The current study was neither designed not powered to address possible effects of co-morbidities and medications on the findings. Interpretation is tempered due to the extremely low sample size for these subgroup analyses. This being an exploratory study, we did not correct for multiple comparisons. We did not measure all possible types of oxidative stress markers. Lastly, BIS-11 scores were only collected from a subset of participants, hence the significant correlation with lower glutathione merits replication in a larger sample, before they can be regarded as firm.
In summary, in this pilot work we found that approximately one-third of adult individuals with trichotillomania had glutathione levels below the normal range; and that lower glutathione was associated with higher motor impulsiveness. Future research should replicate these findings in a larger sample, incorporating a matched internal normal control group, and ideally should dissect the extent to which effects of NAC on brain function and impulsivity are due to glutamatergic versus antioxidant effects (or both). Studies should also examine effects of co-morbidities and various treatments; including whether trichotillomania patients with low baseline levels of glutathione are more likely to experience significant symptom reduction with NAC, which we would hypothesize. The findings may have broader therapeutic relevance for other impulsive and compulsive disorders.