1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). Washington DC: American Psychiatric Publishing; 2013.
2. Salkovskis PM, Wroe AL, Gledhill A, Morrison N, Forrester E, Richards C, et al. Responsibility attitudes and interpretations are characteristic of obsessive compulsive disorder. Behav Res Ther 2000;38:347-372.


4. Pena-Garijo J, Edo Villamón S, Meliá de Alba A, Ruipérez MÁ. Personality disorders in obsessive-compulsive disorder: a comparative study versus other anxiety disorders. Scientific World Journal [Internet]. 2013. Available at:
https://doi.org/10.1155/2013/856846. Accessed May 10, 2019.


5. Friborg O, Martinussen M, Kaiser S, Øvergård KT, Rosenvinge JH. Comorbidity of personality disorders in anxiety disorders: a meta-analysis of 30 years of research. J Affect Disord 2013;145:143-155.


6. Starcevic V, Brakoulias V. New diagnostic perspectives on obsessivecompulsive personality disorder and its links with other conditions. Curr Opin Psychiatry 2014;27:62-67.


7. Gordon OM, Salkovskis PM, Oldfield VB, Carter N. The association between obsessive compulsive disorder and obsessive compulsive personality disorder: Prevalence and clinical presentation. Br J Clin Psychol 2013;52:300-315.


8. Beck JS. Complex cognitive therapy treatment for personality disorder patients. Bull Menninger Clin 1998;62:170-194.

9. Fricke S, Moritz S, Andresen B, Jacobsen D, Kloss M, Rufer M, et al. Do personality disorders predict negative treatment outcome in obsessive-compulsive disorders? A prospective 6-month follow-up study. Eur Psychiatry 2006;21:319-324.


11. Lochner C, Fineberg NA, Zohar J, Van Ameringen M, Juven-Wetzler A, Altamura AC, et al. Comorbidity in obsessive-compulsive disorder (OCD): a report from the International College of Obsessive-Compulsive Spectrum Disorders (ICOCS). Compr Psychiatry 2014;55:1513-1519.


12. Hofmeijer-Sevink MK, Van Oppen P, Van Megen HJ, Batelaan NM, Cath DC, Van Der Wee NJA, et al. Clinical relevance of comorbidity in obsessive compulsive disorder: The Netherlands OCD Association study. J Affect Disord 2013;150:847-854.


13. Crino RD, Andrews G. Obsessive-compulsive disorder and axis I comorbidity. J Anxiety Disord 1996;10:37-46.

14. Beck AT, Beck JS. The Personality Belief Questionnaire. Unpublished Assessment Instrument. Pennsylvania: The Beck Institute for Cognitive Therapy and Research, Bala Cynwyd; 1991.
15. Turkcapar MH, Orsel S, Ugurlu M, Sargin E, Turhan M, Akkoyunlu S, et al. Reliability and validity of Turkish version of Personality Belief Questionnaire. J Clin Psychiatry 2007;10:177-191.
16. Butler AC, Beck AT, Cohen LH. The personality belief questionnaire-short form: Development and preliminary findings. Cognit Ther Res 2007;31:357-370.


17. Taymur I, Turkcapar MH, Orsel S, Sargin E. Validity and reliability of the Turkish cersion of the Personality Belief Questionnaire- Short Form (PBQ-STF) in the university students. J Clin Psychiatry 2011;14:199-209.
18. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006-1011.


19. Tek C, Ulugˇ B, Rezaki BG, Tanriverdi N, Mercan S, Demir B, et al. Yale‐Brown Obsessive Compulsive Scale and US National Institute of Mental Health Global Obsessive Compulsive Scale in Turkish: reliability and validity. Acta Psychiatr Scand 1995;91:410-413.


20. Hisli N. Reliability and validity of Beck Depression Inventory among university students. Turk J Psychol 1989;7:3-13.
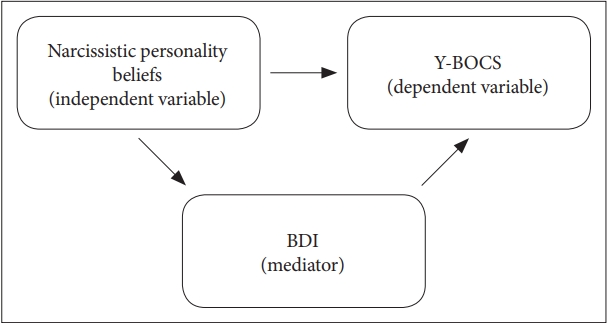
22. Rees CS, Roberts LD, van Oppen P, Eikelenboom M, Hendriks AAJ, van Balkom AJLM, et al. Personality and symptom severity in Obsessive-Compulsive Disorder: the mediating role of depression. Pers Individ Dif 2014;71:92-97.

23. Starcevic V, Brakoulias V. Current understanding of the relationships between obsessive-compulsive disorder and personality disturbance. Curr Opin Psychiatry 2017;30:50-55.


25. Melca IA, Yücel M, Mendlowicz MV, de Oliveira-Souza R, Fontenelle LF. The correlates of obsessive-compulsive, schizotypal, and borderline personality disorders in obsessive-compulsive disorder. J Anxiety Disord 2015;33:15-24.


26. Ansell EB, Pinto A, Edelen MO, Markowitz JC, Sanislow CA, Yen S, et al. The association of personality disorders with the prospective 7-year course of anxiety disorders. Psychol Med 2011;41:1019-1028.


27. Thiel N, Hertenstein E, Nissen C, Herbst N, Külz AK, Voderholzer U. The effect of personality disorders on treatment outcomes in patients with obsessive-compulsive disorders. J Pers Disord 2013;27:697-715.


28. Brakoulias V, Starcevic V, Belloch A, Brown C, Ferrao YA, Fontenelle LF, et al. Comorbidity, age of onset and suicidality in obsessive-compulsive disorder (OCD): An international collaboration. Compr Psychiatry 2017;76:79-86.


30. Dèttore D, Pozza A, Coradeschi D. Does time-intensive ERP attenuate the negative impact of comorbid personality disorders on the outcome of treatment-resistant OCD? J Behav Ther Exp Psychiatry 2013;44:411-417.