1. Gross JJ. Emotion Regulation: Conceptual and Empirical Foundations. In: Gross JJ, editor. Handbook of Emotion Regulation. 2nd Ed. New York, NY: Guilford Publications, 2014, p. 3-20.
2. Cole PM, Michel MK, OŌĆÖ L, Teti D. The Development of Emotion Regulation and Dysregulation: A Clinical Perspective. In: Fox NA, editor. The Development of Emotion Regulation: Biological and Behavioral Considerations. Chicago, IL: University of Chicago Press, 1994, p. 73-100.
3. Gross JJ. The emerging field of emotion regulation: An integrative review. Rev Gen Psychol 1998;2:271-299.

4. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 2003;85:348-362.


5. Gross JJ. Antecedent and response focused emotion regulation: divergent consequences for experience, expression, and physiology. J Pers Soc Psychol 1998;74:224-237.


6. Hu T, Zhang D, Wang J, Mistry R, Ran G, Wang X. Relation between emotion regulation and mental health: a meta-analysis review. Psychol Rep 2014;114:341-362.


7. Richards JM, Gross JJ. Personality and emotional memory: how regulating emotion impairs memory for emotional events. J Res Pers 2006;40:631-651.

8. Balzarotti S, John OP, Gross JJ. An Italian adaptation of the emotion regulation questionnaire. Eur J Psychol Assess 2010;26:61-67.

9. Cabello R, Salguero JM, Fern├Īndez-Berrocal P, Gross JJ. A Spanish adaptation of the Emotion Regulation Questionnaire. Eur J Psychol Assess 2013;29:234-240.

10. Li CH, Wu JJ. Psychometric evaluation of the Chinese version of the Emotion Regulation Questionnaire in Taiwanese college students. Assessment 2020;27:1300-1309.


11. Kwon H, Yoon KL, Joormann J, Kwon JH. Cultural and gender differences in emotion regulation: relation to depression. Cogn Emot 2013;27:769-782.


12. Yang E, Ha J. The mediating effect on perfectionistic self-presentation between emotion suppression and interpersonal problems in university students. Korean J Youth Stud 2020;27:379-403.

13. Spaapen DL, Waters F, Brummer L, Stopa L, Bucks RS. The Emotion Regulation Questionnaire: validation of the ERQ-9 in two community samples. Psychol Assess 2014;26:46-54.


14. Balzarotti S. The emotion regulation questionnaire: factor structure and measurement invariance in an Italian sample of community dwelling adults. Curr Psychol 2019;40:1-12.

15. Wiltink J, Glaesmer H. Regulation of emotions in the community: suppression and reappraisal strategies and its psychometric properties. GMS Psycho Soc Med 2011;8:1-12.
16. Sala MN, Molina P, Abler B, Kessler H, Vanbrabant L, van de Schoot R. Measurement invariance of the Emotion Regulation Questionnaire (ERQ). A cross-national validity study. Eur J Dev Psychol 2012;9:751-757.

17. Fernando SC, Beblo T, Schlosser N, Terfehr K, Otte C, L├Čwe B, et al. The impact of self-reported childhood trauma on emotion regulation in borderline personality disorder and major depression. J Trauma Assoc 2014;15:384-401.

18. Blalock DV, Kashdan TB, Farmer AS. Trait and daily emotion regulation in social anxiety disorder. Cogn Ther Res 2016;40:416-425.

19. Fitzgerald JM, MacNamara A, Kennedy AE, Rabinak CA, Rauch SA, Liberzon I, et al. Individual differences in cognitive reappraisal use and emotion regulatory brain function in combat-exposed veterans with and without PTSD. Depress Anxiety 2017;34:79-88.


20. Moran EK, Culbreth AJ, Barch DM. Emotion regulation predicts everyday emotion experience and social function in schizophrenia. Clin Psychol Sci 2018;6:271-279.


21. Hannan SM, Orcutt HK. Emotion regulation in undergraduate students with posttraumatic stress symptoms: a multimethod study. Psychol Trauma 2020;12:643-650.


22. Khan AJ, Maguen S, Straus LD, Nelyan TC, Gross JJ, Cohen BE. Expressive suppression and cognitive reappraisal in veterans with PTSD: results from the mind your heart study. J Affect Disord 2021;283:278-284.


23. Nagulendran A, Jobson L. Exploring cultural differences in the use of emotion regulation strategies in posttraumatic stress disorder. Eur J Psychotraumatol 2020;11:1-11.

24. Post LM, Youngstrom E, Connell AM, Zoellner LA, Feeny NC. Transdiagnostic emotion regulation processes explain how emotion-related factors affect co-occurring PTSD and MDD in relation to trauma. J Anxiety Disord 2021;78:102367


25. Naumann E, Svaldi J. Influence of suppression and reappraisal on eating-related symptoms and ruminative thinking in anorexia nervosa and bulimia nervosa. Behav Res Ther 2021;141:103851


26. Meule A, Richard A, Schnepper R, Reichenberger J, Georgii C, Naab S, et al. Emotion regulation and emotional eating in anorexia nervosa and bulimia nervosa. Eat Disord 2021;29:175-191.

27. Aslan IH, Baldwin DS. Ruminations and their correlates in depressive episodes: between-group comparison in patients with unipolar or bipolar depression and healthy controls. J Affect Disord 2021;280:1-6.

28. Kivity Y, Cohen L, Weiss M, Elizur J, Huppert JD. The role of expressive suppression and cognitive reappraisal in cognitive behavioral therapy for social anxiety disorder: a study of self-report, subjective, and electrocortical measures. J Affect Disord 2021;279:334-342.


29. Ferreira S, Couto B, Sousa M, Vieira R, Sousa N, Pic├│-P├®rez M, et al. Stress influences the effect of obsessive-compulsive symptoms on emotion regulation. Front Psychiatry 2021;11:594511

30. Marco JH, Fernandez-Felipe I, Fonseca S, Garcia-Palacios A, Ba├▒os R, Guillen V. Confirmatory factor analysis and psychometric properties of the Emotion Regulation Questionnaire in participants with personality disorders. Clin Psychol Psychother 2021;28:1598-1606.


31. Lee M, Lee ES, Jun JY, Park S. The effect of early trauma on North Korean refugee youthsŌĆÖ mental health: moderating effect of emotional regulation strategies. Psychiatry Res 2020;287:112707


32. Oh DH, Lee S, Kim SH, Ryu V, Cho HS. Low working memory capacity in euthymic bipolar I disorder: no relation to reappraisal on emotion regulation. J Affect Disord 2019;252:174-181.


33. Lee Y, Kim BN, Park MH, Park S. Familial, cognitive, and behavioral characteristics of adolescents with depression. J Korean Acad Child Adolesc Psychiatry 2017;28:168-173.

34. Kim SH, Cornwell B, Kim SE. Individual differences in emotion regulation and hemispheric metabolic asymmetry. Biol Psychol 2012;89:382-386.


36. Velotti P, Rogier G, Civilla C, Garofalo C, Serafini G, Amore M. Dysregulation of positive emotions across community, clinical and forensic samples using the Italian version of the difficulties in emotion regulation scale-positive (DERS-positive). J Forens Psychiatry Psychol 2020;31:555-570.

37. First MB, Williams JBW, Karg RS, Spitzer RL. UserŌĆÖs Guide for the SCID-5-CV Structured Clinical Interview for DSM-5┬« Disorders: Clinical Version. Arlington, VA: American Psychiatric Publishing, Inc; 2016.
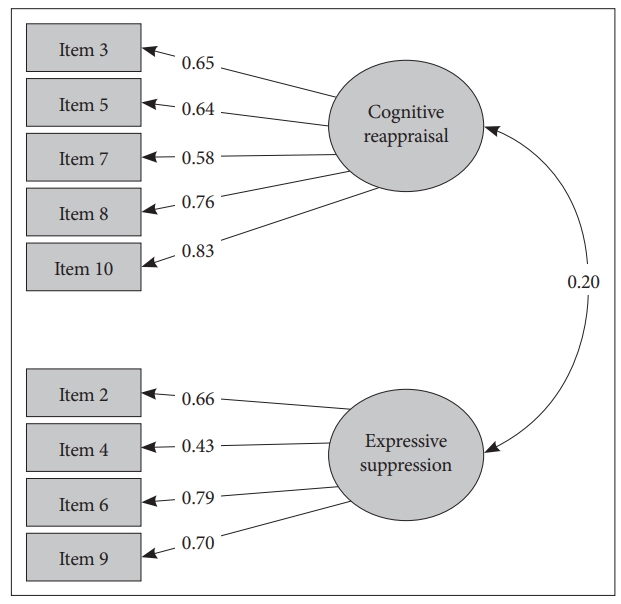
38. Shon J. Individual Differences in Two Regulation Strategies: Cognitive Reappraiser vs. Emotion Suppressor. [dissertation]. Seoul: Seoul National University; 2005.
40. Beck AT, Steer RA, Brown GK. Beck Depression Inventory (BDI-II). San Antonio, TX: Psychological Corporation; 1996.
41. Lim SU, Lee EH, Hwang ST, Hong SH, Kim JH. Psychometric Properties of the Beck Depression Inventory-II in Korea. Poster presented at: Fall Conference of the Korean Clinical Psychology Association 2014;Korea.
42. Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess 2007;19:176-188.


44. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 2015;28:489-498.


45. Kim JW, Chung HG, Choi JH, So HS, Kang SH, Kim DS, et al. Psychometric properties of the Korean version of the PTSD Checklist-5 in elderly Korean veterans of the Vietnam war. Anxiety Mood 2017;13:123-131.
46. Joe KH, Chai SH, Park A, Lee HK, Shin IH, Min SH. Optimum cut-off score for screening of hazardous drinking using the Korean version of alcohol use disorder identification test (AUDIT-K). J Korean Acad Addict Psychiatry 2009;13:34-40.
47. Kline RB. Principles and Practice of Structural Equation Modeling. 4th ed. New York, NY: Guilford Publications; 2015.
48. Muth├®n LK, Muth├®n BO. Mplus UserŌĆÖs Guide. 7th ed. Los Angeles, CA: Muth├®n & Muth├®n; 1998.
49. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1-55.

50. Brown MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res 1992;21:230-258.

51. IMB Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013.
52. DeVellis RF. Scale Development Theory and Applications. 2nd ed. Los Angeles, LA: SAGE Publications; 2003.
54. Preece DA, Becerra R, Hasking P, McEvoy PM, Boyes M, Sauer-Zavala S, et al. The emotion regulation questionnaire: psychometric proper ties and relations with affective symptoms in a United States general community sample. J Affect Disord 2021;284:27-30.


55. Mohammed AR, Kosonogov V, Lyusin D. Expressive suppression versus cognitive reappraisal: effects on self-report and peripheral psychophysiology. Int J Psychophysiol 2021;167:30-37.


56. Butler EA, Egloff B, Wilhelm FH, Smith NC, Erickson EA, Gross JJ. The social consequences of expressive suppression. Emotion 2003;3:48-67.


57. Sheppes G. Emotion Regulation Choice: Theory and Findings. In: Gross JJ, editor. Handbook of Emotion Regulation. 2nd ed. New York, NY: Guilford Publications, 2014, p. 126-139.
58. Haga SM, Kraft P, Corby EK. Emotion regulation: antecedents and well-being outcomes of cognitive reappraisal and expressive suppression in cross-cultural samples. J Happiness Stud 2009;10:271-291.

59. Melka SE, Lancaster SL, Bryant AR, Rodriguez BF. Confirmatory factor and measurement invariance analyses of the emotion regulation questionnaire. J Clin Psychol 2011;67:1283-1293.


60. Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion 2006;6:587-595.


61. Beblo T, Fernando S, Klocke S, Griepenstroh J, Aschenbrenner S, Driessen M. Increased suppression of negative and positive emotions in major depression. J Affect Disord 2012;141:474-479.


62. DŌĆÖAvanzato C, Joormann J, Siemer M, Gotlib IH. Emotion regulation in depression and anxiety: examining diagnostic specificity and stability of strategy use. Cognit Ther Res 2013;37:968-980.

65. Shushakova A, Ohrmann P, Pedersen A. Exploring deficient emotion regulation in adult ADHD: electrophysiological evidence. Eur Arch Psychiatry Clin Neurosci 2018;268:359-371.


67. Boden MT, Gross JJ, Babson KA, Bonn-Miller MO. The interactive effects of emotional clarity and cognitive reappraisal on problematic cannabis use among medical cannabis users. Addict Behav 2013;38:1663-1668.


68. Perez CR, Soto JA. Cognitive reappraisal in the context of oppression: implications for psychological functioning. Emotion 2011;11:675-680.


70. Chung MC, Shakra M, AlQarni N, AlMazrouei M, Al Mazrouei S, Al Hashimi S. Posttraumatic stress among Syrian refugees: trauma exposure characteristics, trauma centrality, and emotional suppression. Psychiatry 2018;81:54-70.